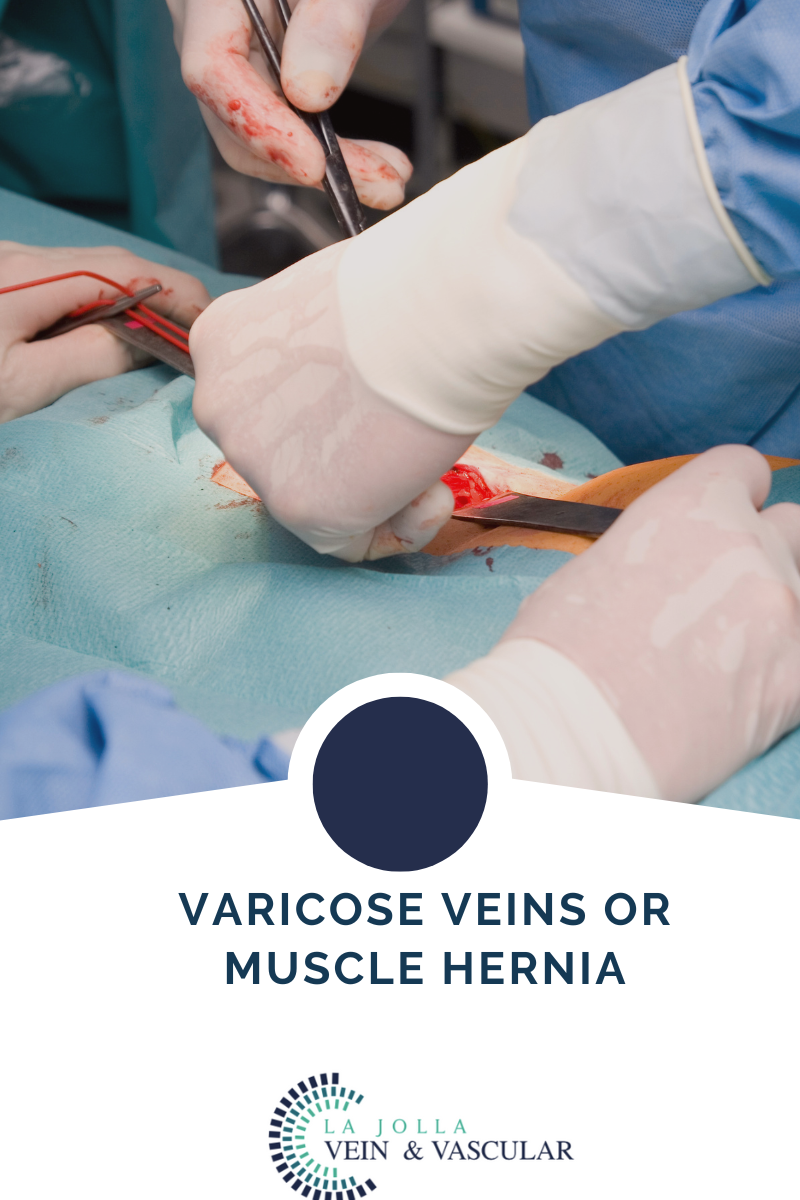
Varicose veins or muscle hernia?
LJVascular2022-07-20T16:14:11-07:00A muscle hernia of the legs is frequently confused with varicose veins. Patients may present with bulging along the outer part of the shin, that looks like a varicose vein. It may or may not be painful. It goes away with flexing the foot (pointing your toes to your head). But, to experienced […]