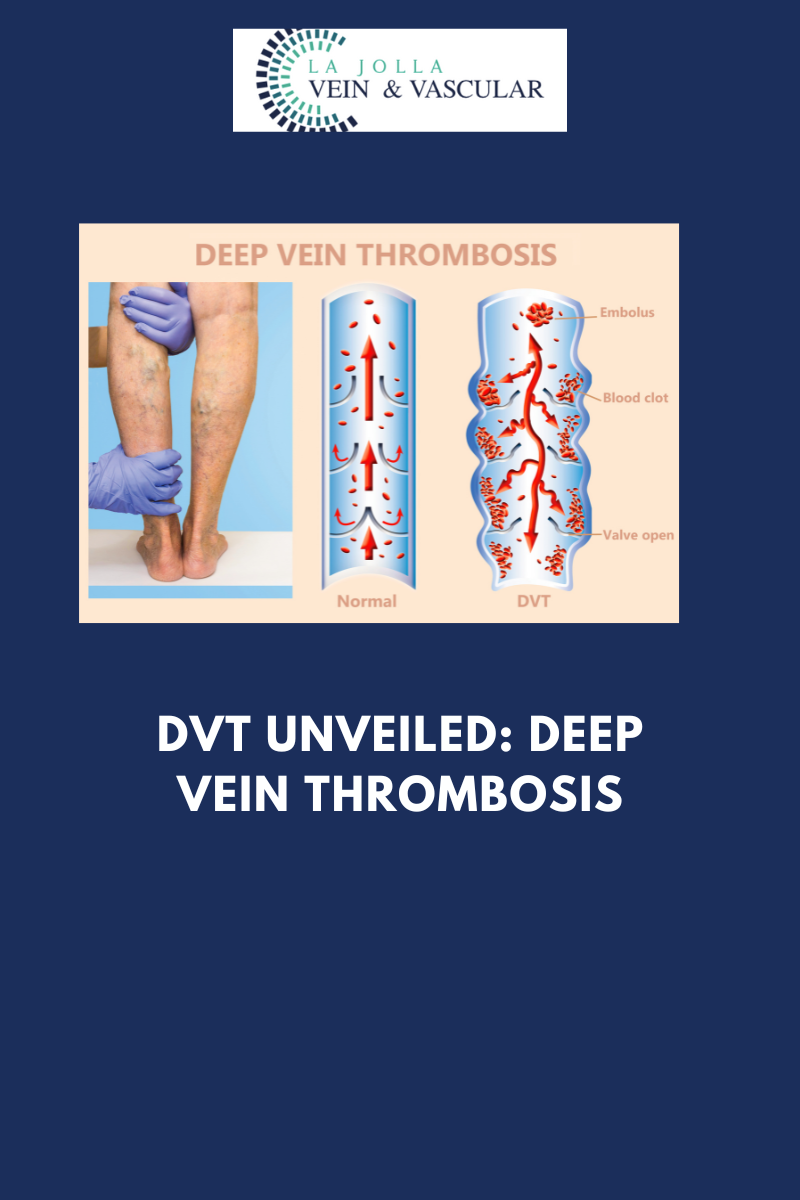
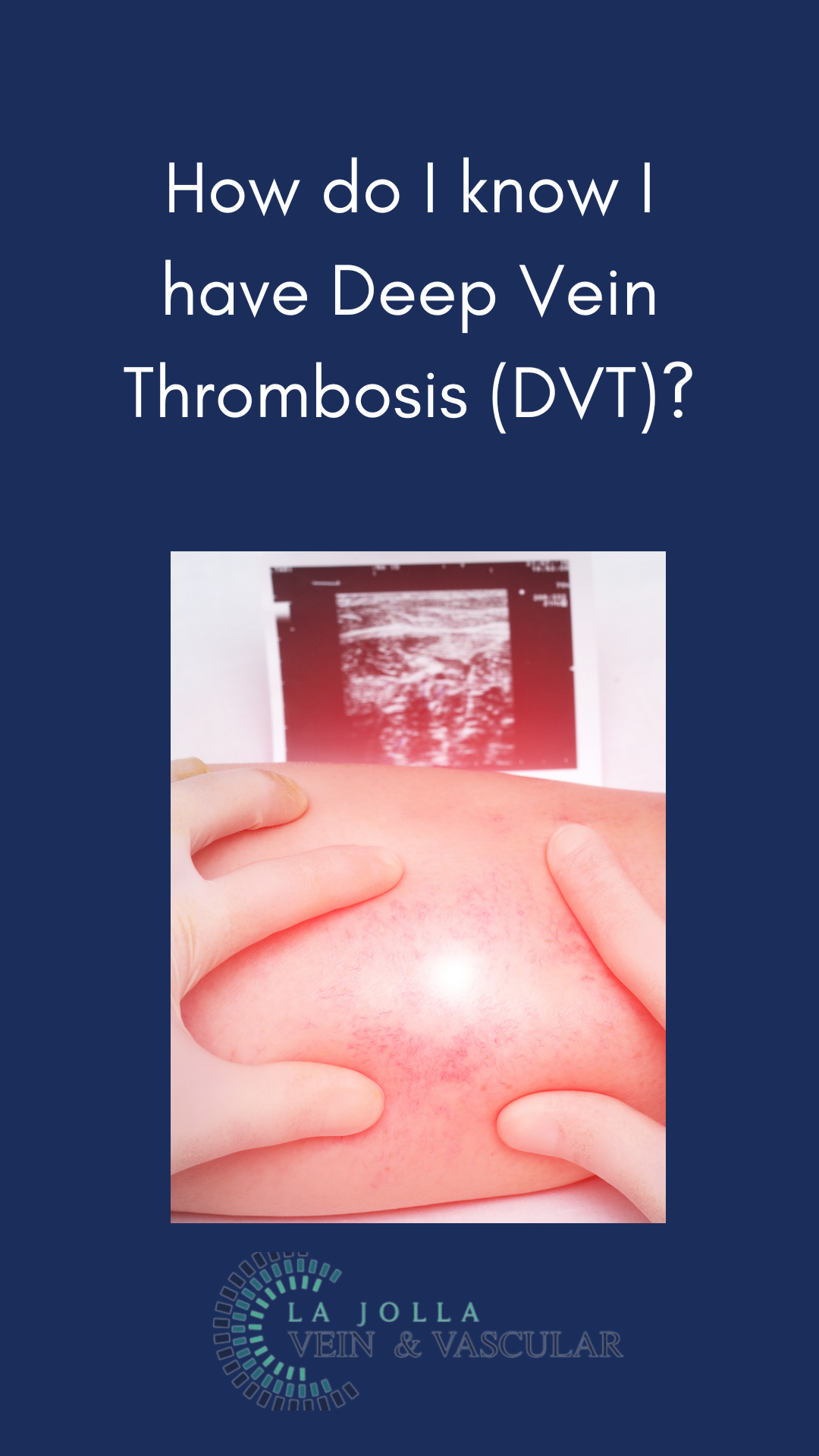
DVT Unveiled: Deep Vein Thrombosis
LJVascular2024-10-24T20:16:52-07:00DVT Unveiled: Deep Vein Thrombosis
Deep Vein Thrombosis (DVT) may not always be visible on the surface, but its potential consequences are far from hidden. In this blog post, we’ll explore what DVT is, why it’s a serious medical condition, how it can be diagnosed, and the importance of vigilance in its […]