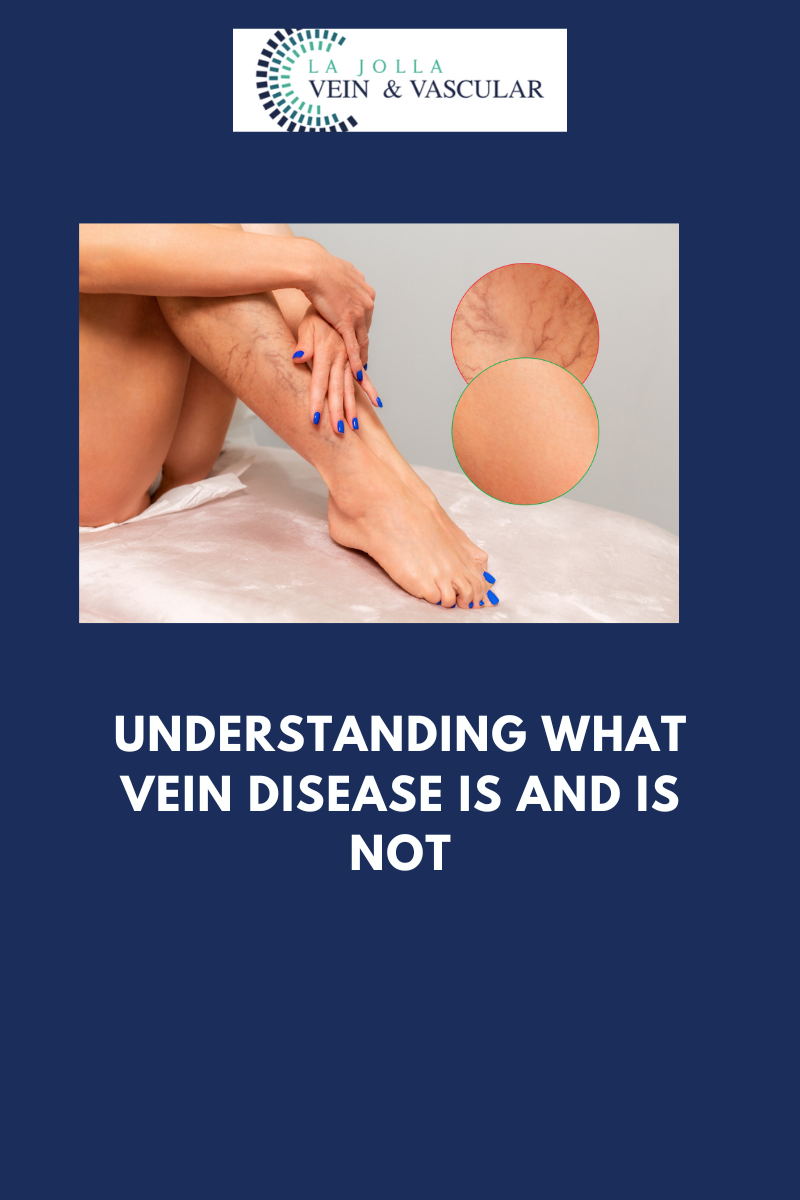
Understanding what vein disease is and is not
LJVascular2023-08-29T18:44:36-07:00Understanding what vein disease is and is not
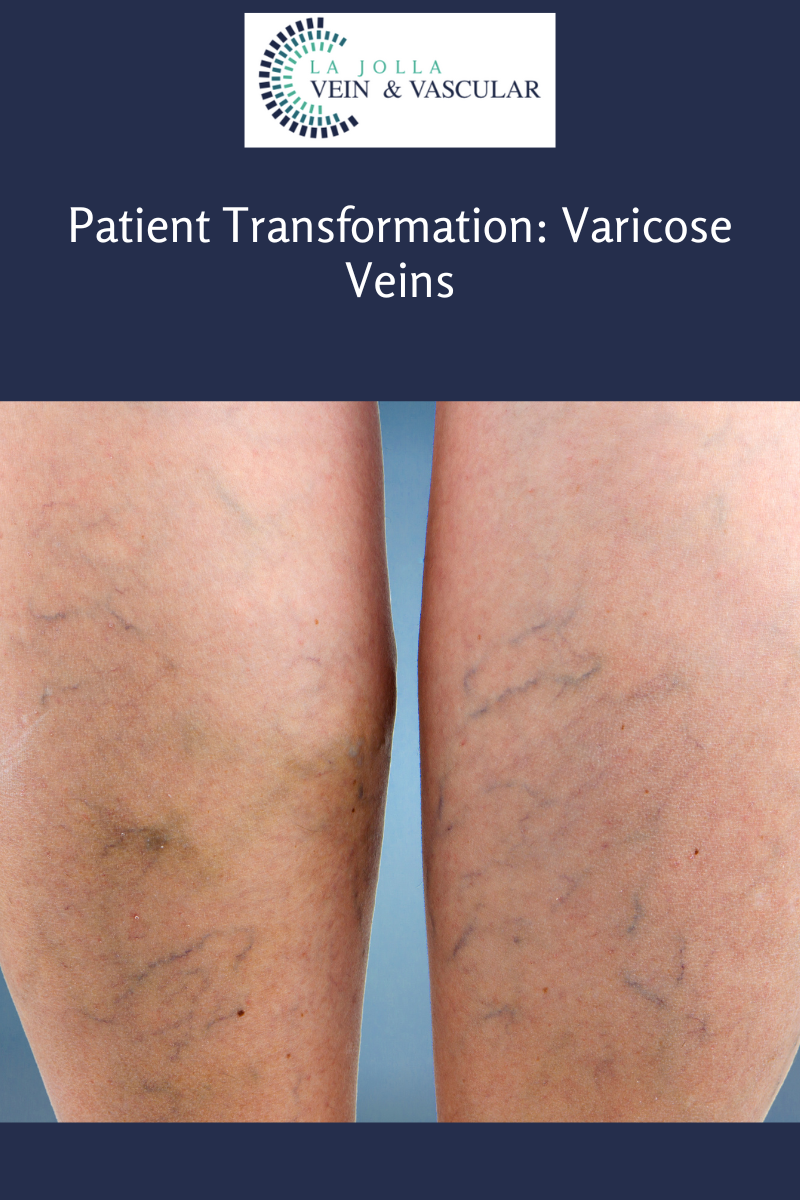
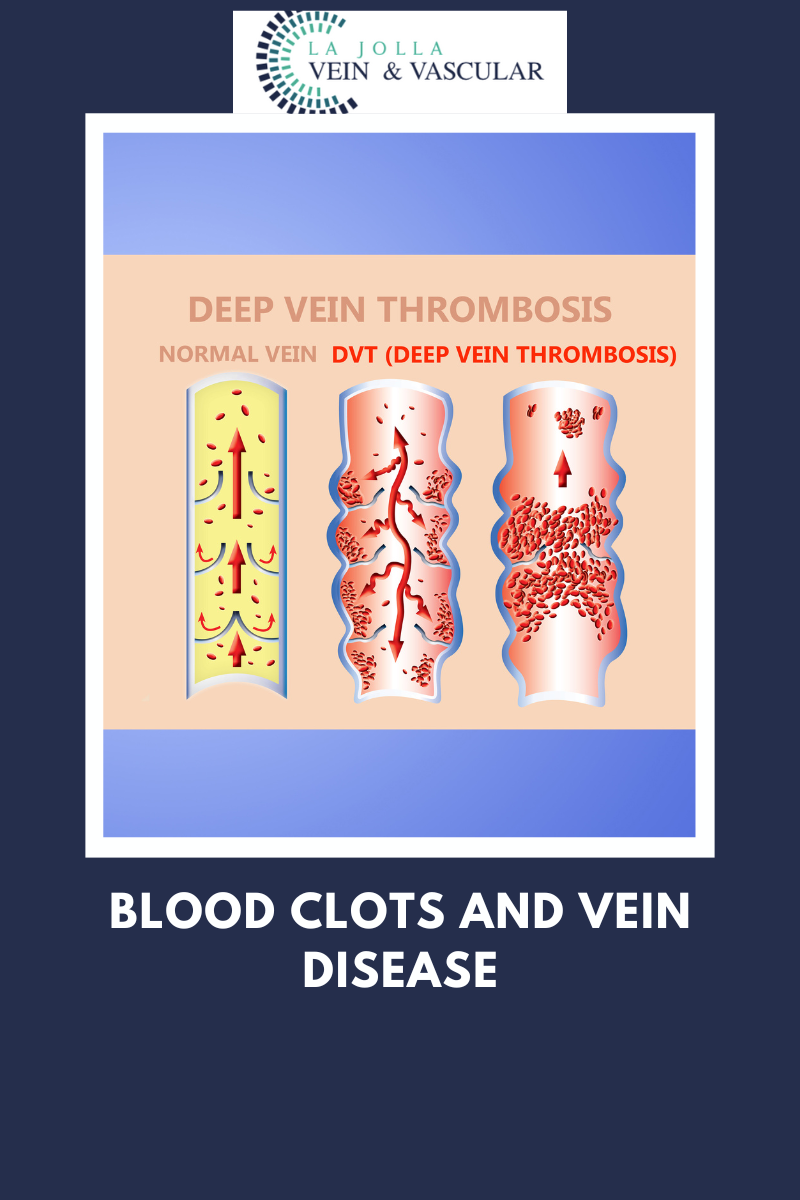
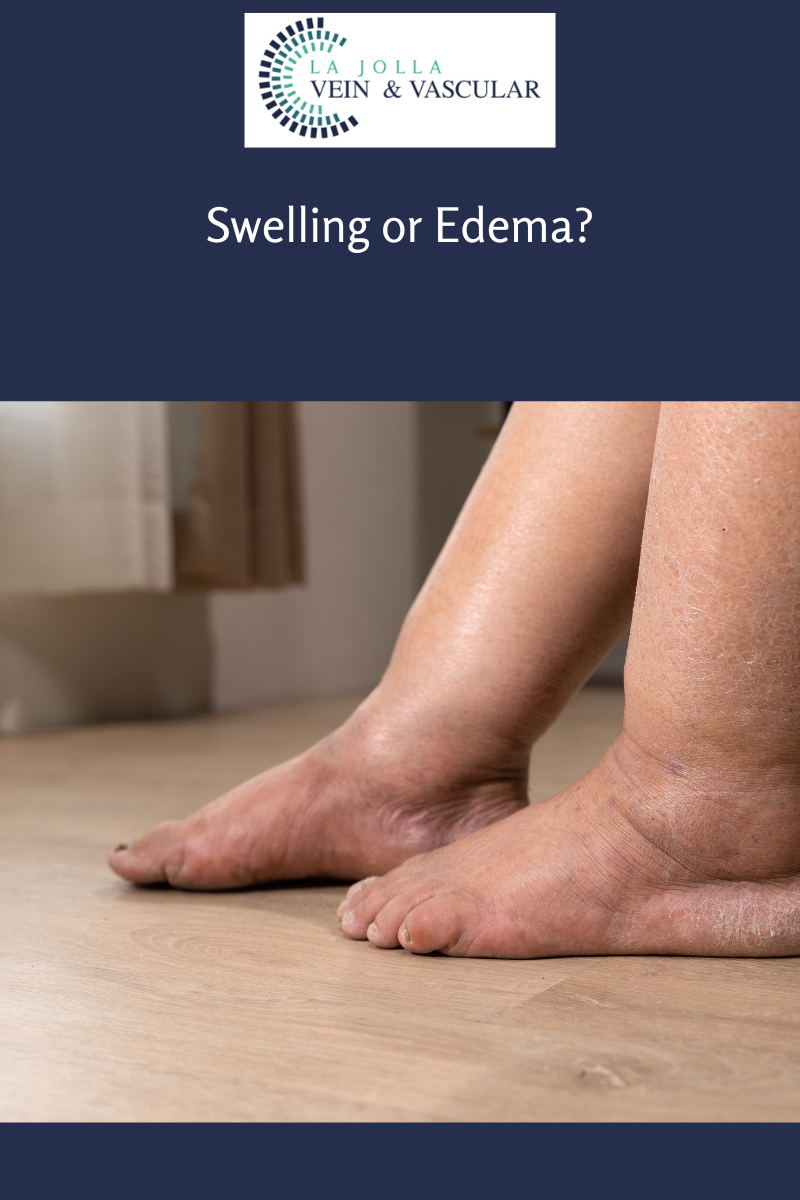
Venous reflux disease, alternatively referred to as venous stasis, venous insufficiency, or venous incompetence, is a complex condition affecting the veins of the legs. In this article, we will delve into the details of venous reflux disease, from its causes and symptoms to the […]