What is Venous Reflux Disease?
LJVascular2022-03-17T10:21:46-07:00What is Venous Reflux Disease?
Venous reflux disease is also known as venous stasis, venous insufficiency or venous incompetence and refers to ‘leaky valves’ in the veins of the legs.
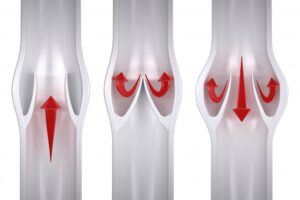
Reflux may occur in the deep and/or superficial leg veins. The deep veins are […]