What is GAE?
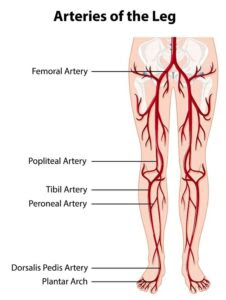
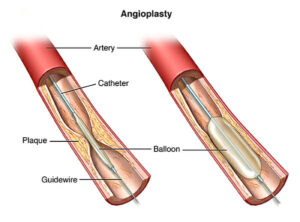
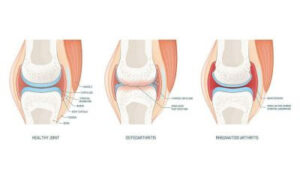
LJVascular2023-05-24T15:26:37-07:00Genicular artery embolization (GAE) is an interventional radiology procedure used to treat knee pain due to osteoarthritis. The procedure minimizes the flow of blood to the knee lining (synovium). Osteoarthritis causes the bones in the knee joint to rub each other, creating friction. This leads to increased flow of blood to the knee due to inflammation. Genicular artery embolization (GAE) is a relatively new and effective minimally invasive procedure that is ideal for people with;
- Mild to severe knee osteoarthritis
- People who have not responded to medication, injections, and therapy
- People who are not read to undergo partial or complete knee replacement surgery
While the procedure does not treat the underlying cartilage damage, it effectively treats the symptoms associated with knee arthritis. Additionally, unlike knee surgery, physical therapy is unnecessary after undergoing the Genicular artery embolization (GAE) procedure.
Why Choose Genicular Artery Embolization (GAE )?
It is essential to point out that while Genicular artery embolization (GAE). It is a relatively new procedure for treating osteoarthritis (OA). It is more effective than other treatments. One of the main reasons you should choose Genicular artery embolization (GAE) is that it is minimally invasive. The procedure is performed by an outpatient surgeon, allowing you to go back home the same day. Research also shows that the procedure has low risk and much faster recovery. Unlike taking drugs with numerous side effects, such as stomach upsets, the procedure has minimal side effects. Additionally, the procedure has a very high success rate, with eighty-five percent of patients treated with Genicular artery embolization (GAE) reporting significant pain and discomfort relief within the first month.
Genicular Artery Embolization (GAE) vs. Surgery
Compared to traditional surgeries performed to treat knee osteoarthritis, Genicular artery embolization (GAE) is more efficient and safe. This procedure is minimally invasive for starters, meaning that it requires a small incision in the skin. The scar is barely visible in 1-2 months after the procedure. No one loves having scars on their feet. Unfortunately, extensive knee surgeries such as complete knee replacement leave large scars that are difficult to conceal.
Secondly, you get to go home the same day. Knee surgeries require the use of general/local anesthesia, which takes time to wear off. You will also need to spend a night or two for doctor observation after surgery. With Genicular artery embolization (GAE), you do not need to spend the night in the medical facility. Additionally, the procedure works for everyone, including people at high risk of complications and would not want to undergo expensive knee surgeries.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!