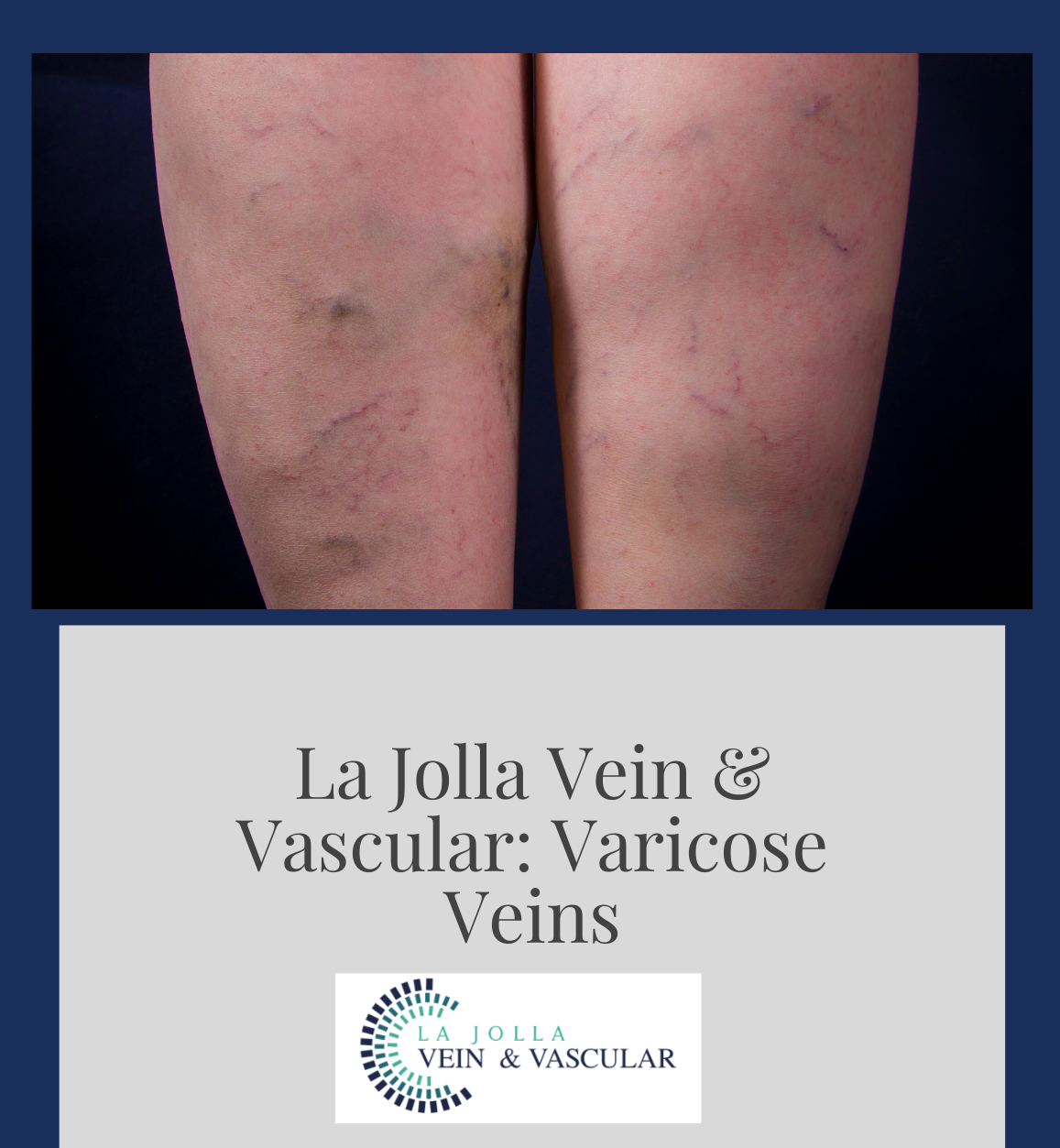
Ways to treat varicose veins without procedures
LJVascular2022-10-24T11:24:45-07:00Ways to treat varicose veins without procedures: conservative management and self-care.
Conservative Management and Self-Care for Varicose Veins
Conservative management and lifestyle changes can ease the symptoms of varicose veins and help reduce complications such as thrombophlebitis (blood clots within veins) and vein rupture, but do not cause the veins to vanish. These measures are helpful if an individual is not a candidate for vein procedures or wishes to delay interventional treatment. More common options include:
Compression stockings: These elastic stockings squeeze or compress the veins to help circulate blood. The compression stockings prevent blood from flowing backward and pooling in the legs. Compression stockings must be graduated, medical grade compression to be beneficial. TED hose are not adequate to reduce symptoms in venous disease for active patients. Compression stockings come in different strengths and the most common strength for the treatment of varicose veins is 20-30mmhg. Your doctor should advise you which strength of compression stockings you should wear. In patients with peripheral arterial disease (PAD), diabetics, and neuropathies, compression may be contraindicated or lesser strengths of compression may be advised.
Leg elevation: Use leg elevation three or four times a day for about 15 minutes at a time. Even elevating your legs on a step stool or ottoman is beneficial. If you need to sit or stand for a long period of time, flexing (bending) your legs occasionally can help keep blood circulating. If you have mild to moderate varicose veins, elevating your legs can help reduce leg swelling and relieve other symptoms.
Exercise: Exercising is good for your veins because it improves blood flow. Walking, cycling, or swimming are great exercises for vein health. But be sure to check with your doctor before starting any exercise program.
Avoid inactivity: Standing or sitting for long periods of time can aggravate your vein condition. To keep blood moving when you have to sit or stand for long periods, try these tips: at work, take walking breaks and try walking during your lunch hour. While sitting, try flexing your feet up and down 10 times an hour. When standing, raise yourself up and down on your toes or rock back and forth on your heels.
Dietary Supplements: Supplements such as horse chestnut and grape seed extract can help reduce symptoms of venous disease. Vasculera is a prescription medication that may be helpful for some. Always check with your PCP before starting supplements or new medications as there may be side effects.
Dietary Changes and High Fiber Diet: A flavonoid rich diet including berries, and green teas, can reduce inflammation and pain. A high fiber diet can increase abdominal pressure and may be helpful for varicose veins. Make sure to drink plenty of water with your high fiber diet.
Anti-inflammatory Medications: are helpful to reduce pain and inflammation, but check with your doctor first to make sure you don’t have contraindications to using them. Ibuprofen and Advil are common oral anti-inflammatory medications. There are also anti-inflammatory cream or gels that can be applied topically to the painful veins, such as Voltaren gel.
Ice packs: and heating pads can be applied to tender veins. Ice packs and heating pads can be used in an alternating manner.
Weight loss or maintaining a healthy weight: Being overweight puts extra pressure on your veins. It’s optimal to manage your weight to reduce extra symptoms and pain. These are the 9 best ways to treat varicose veins with conservative management.
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link.
For more information on varicose veins and eliminating underlying venous insufficiency, check this link out full of resources.