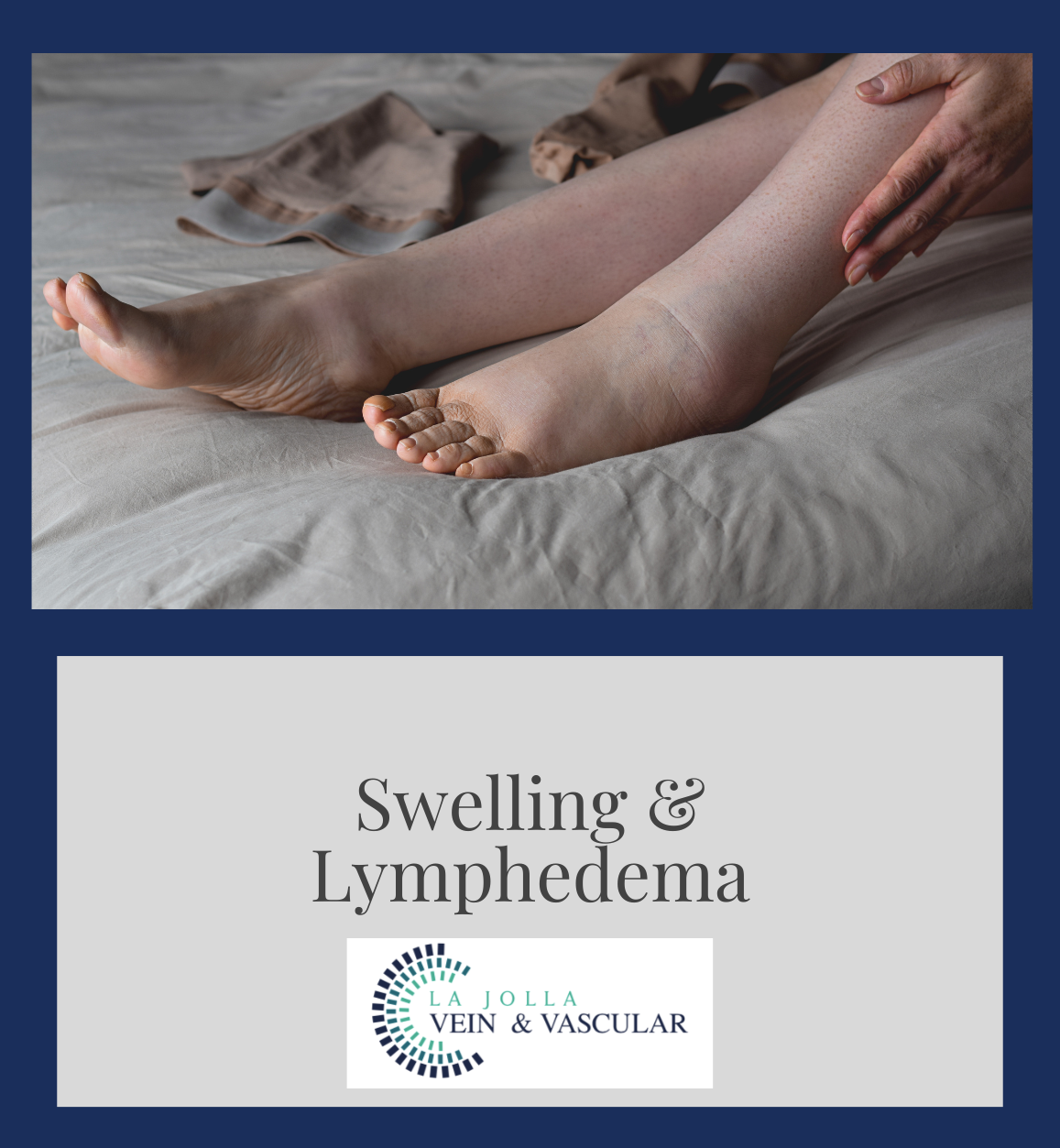
Swelling and Lymphedema
LJVascular2023-01-14T12:59:50-08:00Complications of Untreated Varicose Veins and Venous Insufficiency: Swelling of the Ankles/legs and lymphedema
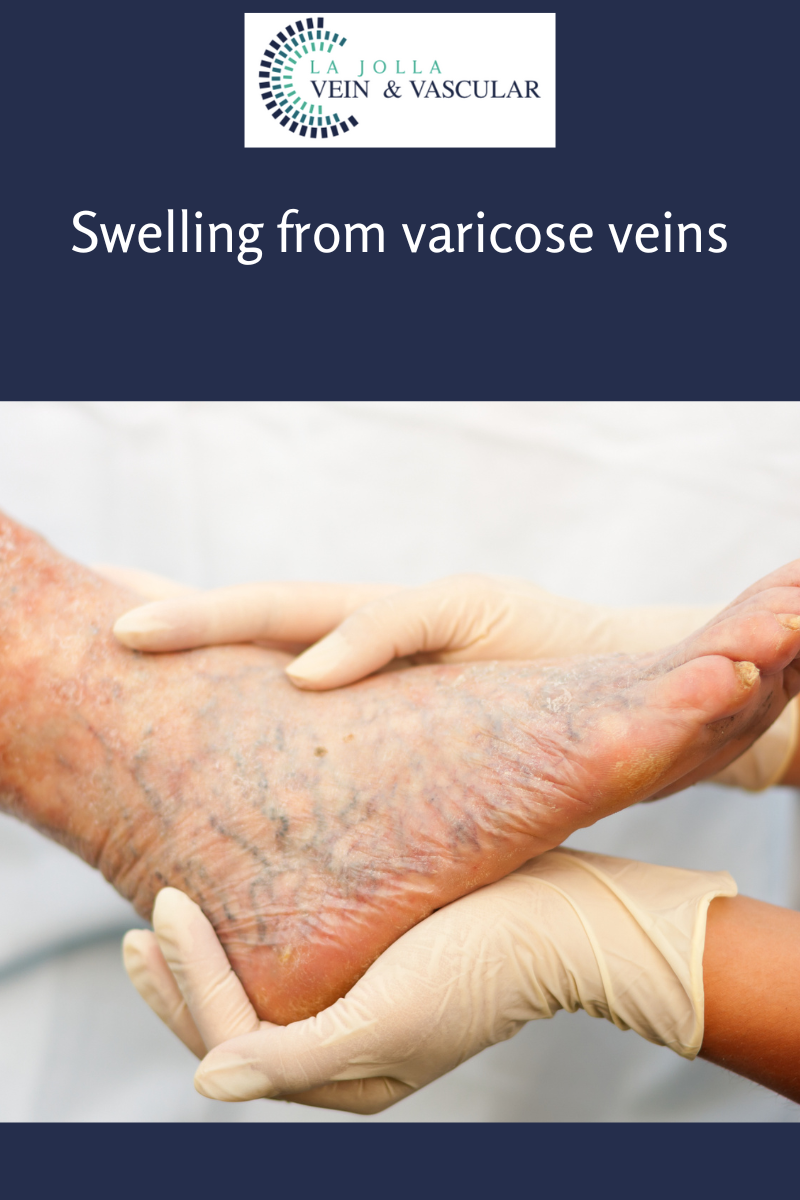
Leg swelling (swelling is also known as edema), is a common complaint related to varicose veins and underlying venous insufficiency. Leg swelling can be present simply from underlying venous insufficiency without visible signs of varicose veins or spider veins. As a result, a venous insufficiency study by duplex ultrasound scanning is part of the recommended work-up for leg swelling.
The Duplex Ultrasound involves using high frequency sound waves to look at the speed of blood flow, and structure of the blood vessels. The term “duplex” refers to the fact that two modes of ultrasound are used, Doppler and B-mode. The B-mode transducer obtains an image of the vessel being studied. The Doppler probe within the transducer evaluates the velocity and direction of blood flow in the vessel.
The swelling usually affects the ankles. Most people with vein-related swelling experience progressive swelling throughout the day, that is worse at night time and improved in the morning (they usually wake up with normal appearing legs in the morning but by night-time, shoes may feel tight.) Vein-related swelling is worse at the end of the day, with prolonged standing, sitting or with air travel, heat and menstruation. The degree of swelling varies from one person to another.
Leg swelling is a common symptom of varicose veins and venous insufficiency. The legs often feel heavy. It is common to notice sock lines around the ankles by the end of the day.
Compression stockings and leg elevation will help reduce swelling. If the swelling can be attributed to the varicose veins or venous insufficiency, correction of the underlying vein problem will reduce swelling.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link.
For more information on varicose veins and eliminating underlying venous insufficiency, check this link out full of resources.
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.