3 Ways to keep your legs looking healthy and beautiful
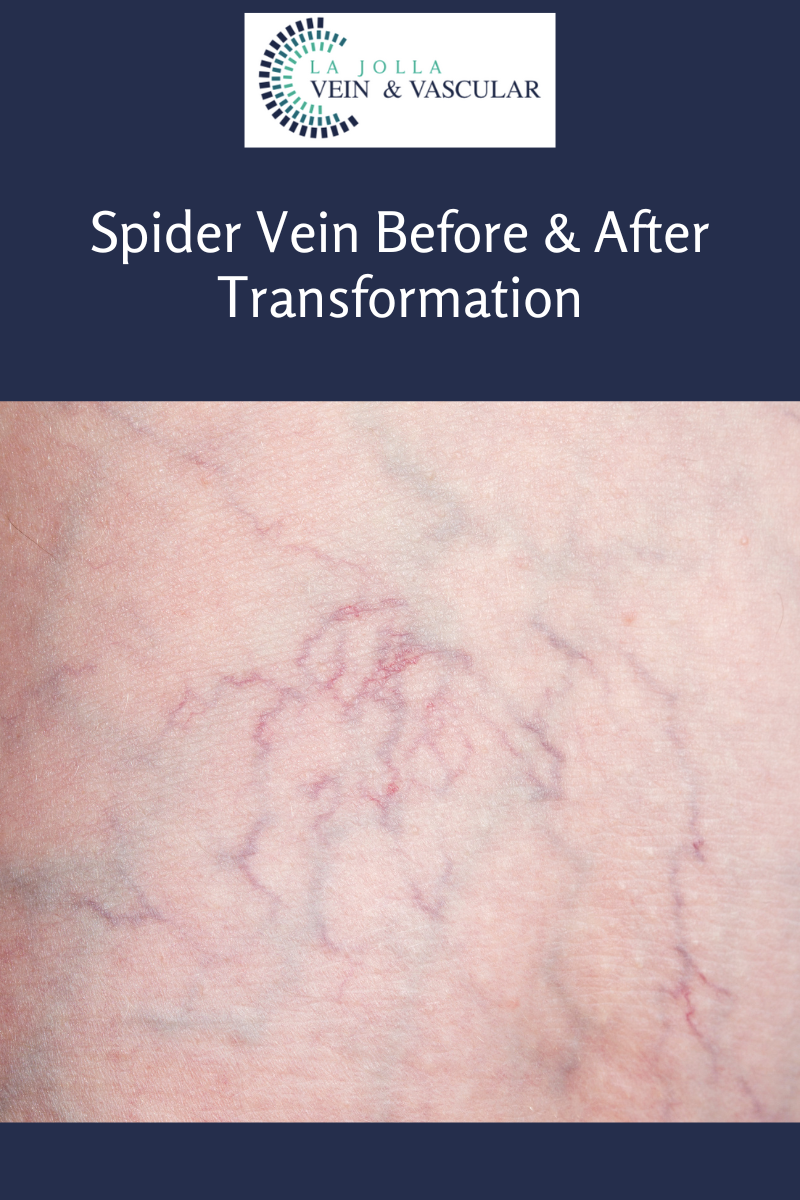
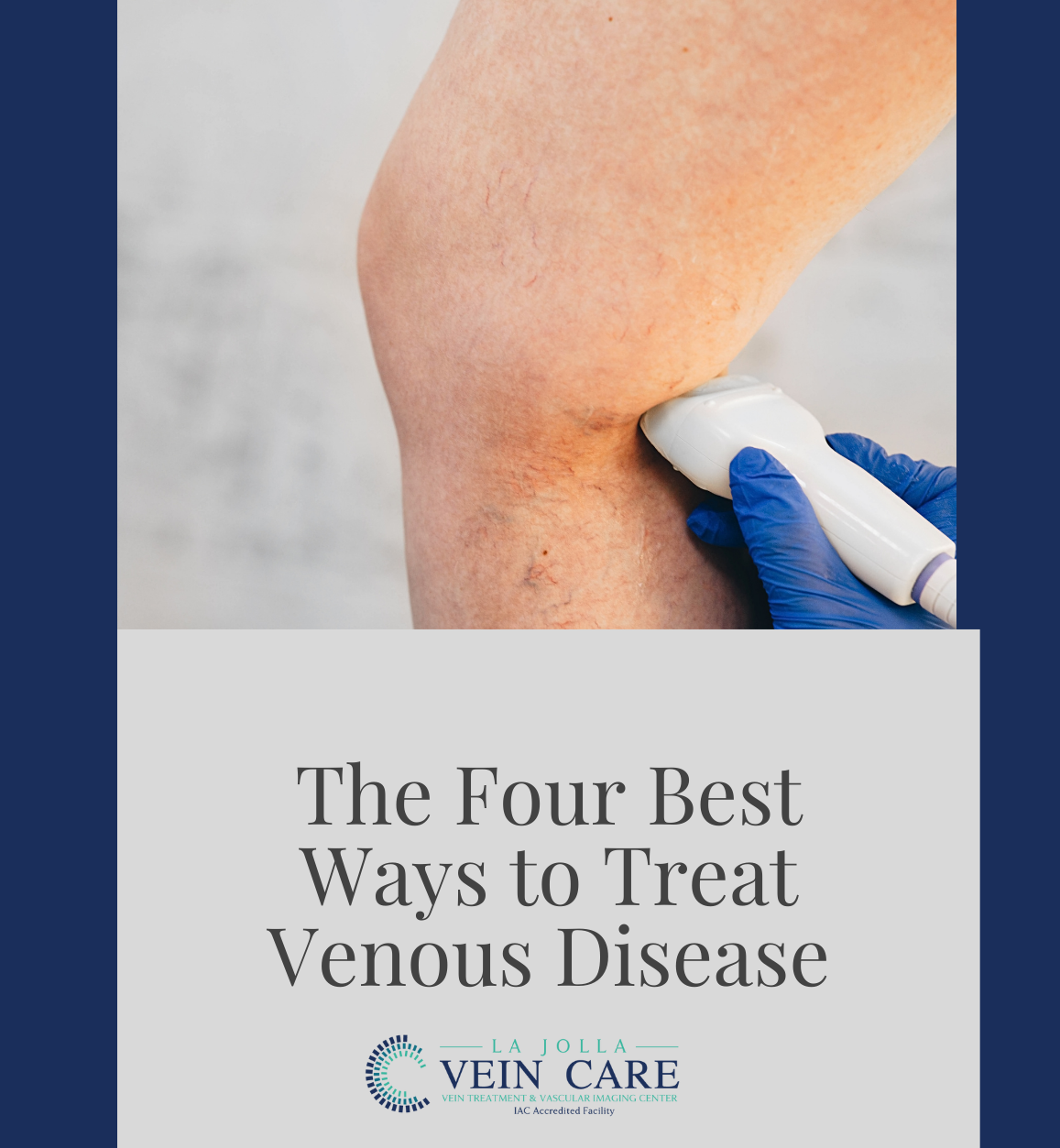
LJVascular2022-07-16T18:16:24-07:00Keeping your legs beautiful might require a little help. Varicose veins, for example, affect a large number of people around the world every year. In the United States alone, up to 55% of women are likely to experience vein-related problems in their legs, which can cause undesirable skin changes. There are three ways […]