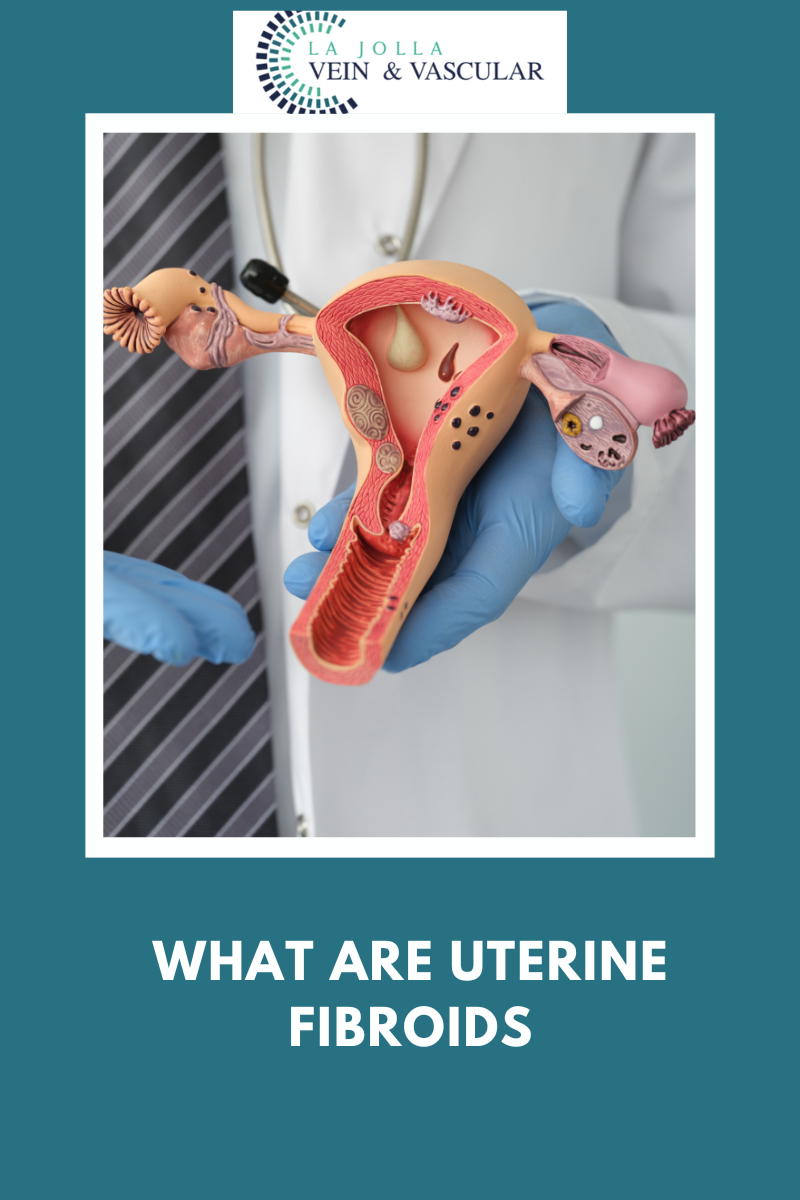
What are uterine fibroids?
LJVascular2023-02-13T17:24:11-08:00Millions of women around the world are affected by the development of uterine fibroids each year. While it is not a life-threatening condition in itself, the symptoms and potential complications that come with it make it such a pressing medical concern for affected individuals.
As only women will usually possess a uterus, […]