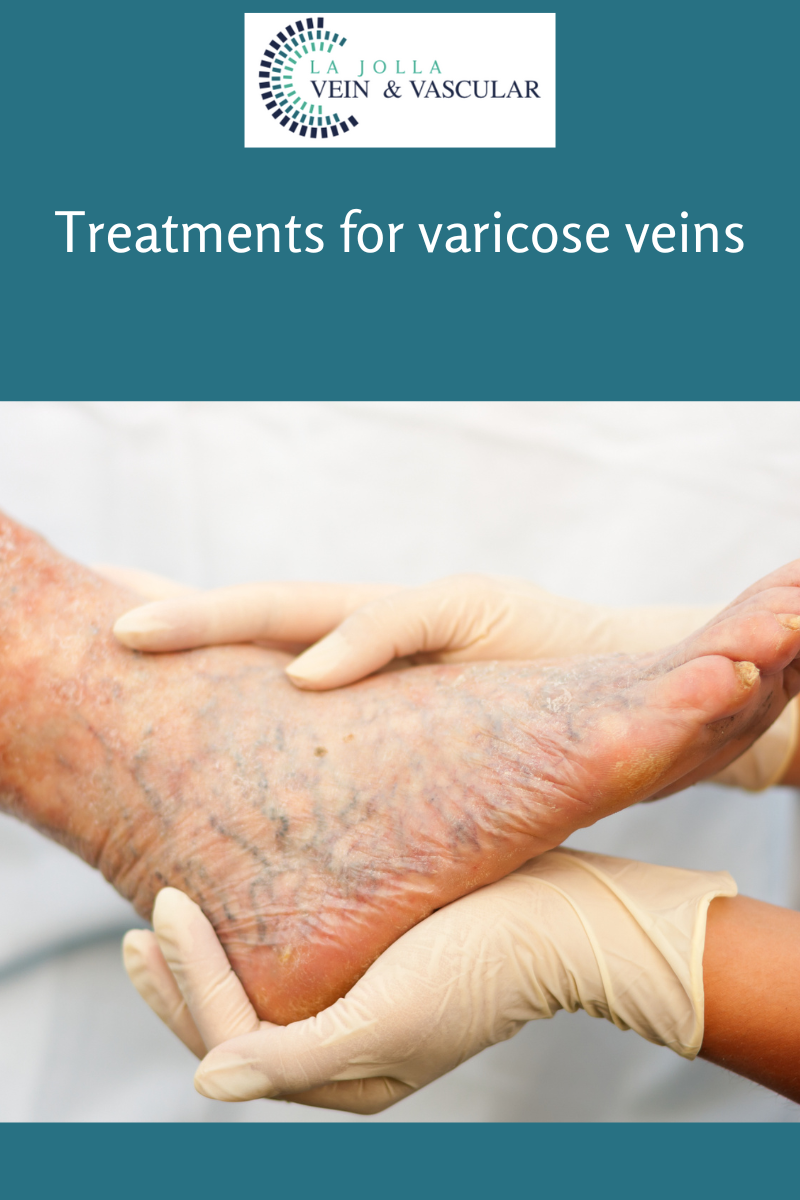
Treatments for varicose veins
LJVascular2023-02-15T18:53:12-08:00Conservative Management & Lifestyle Modifications
The goals of treatment are to relieve symptoms, prevent complications and for some to improve appearance. Lifestyle changes can ease the symptoms, but do not cause the veins to vanish. These treatments include:
- Avoid standing or sitting for long periods of time: […]