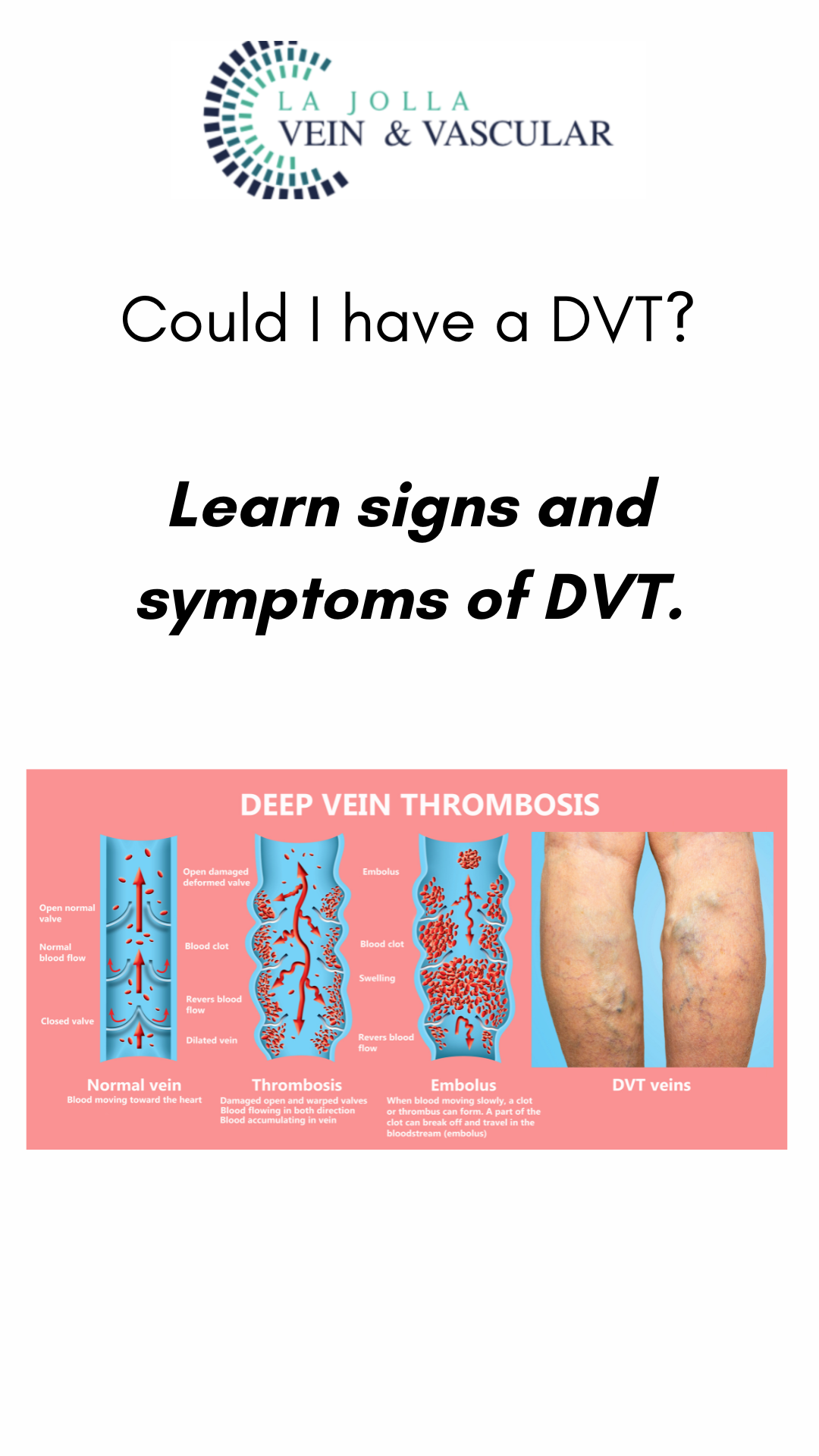
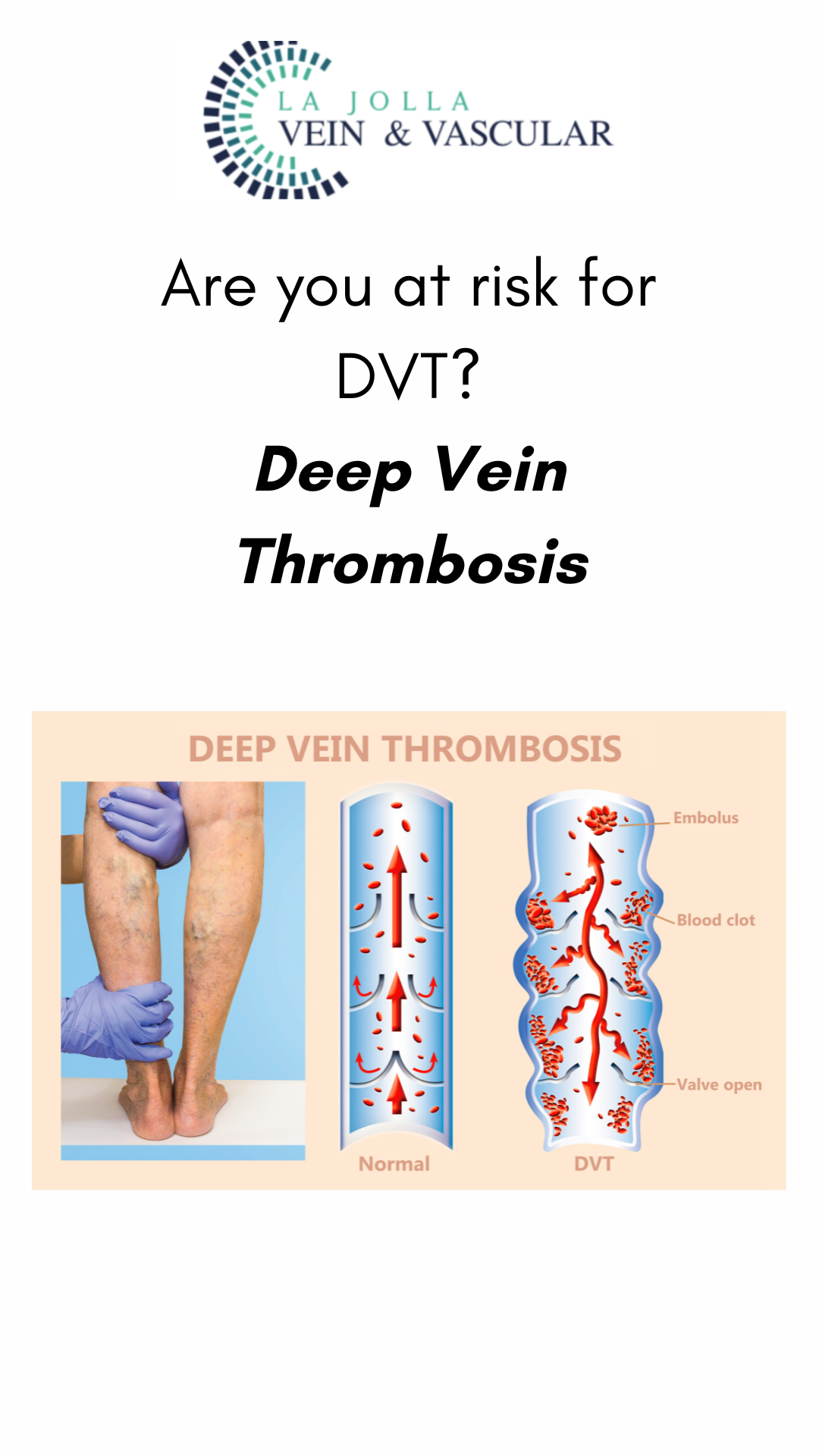
Could I have a DVT? Learn signs and symptoms of Deep Vein Thrombosis
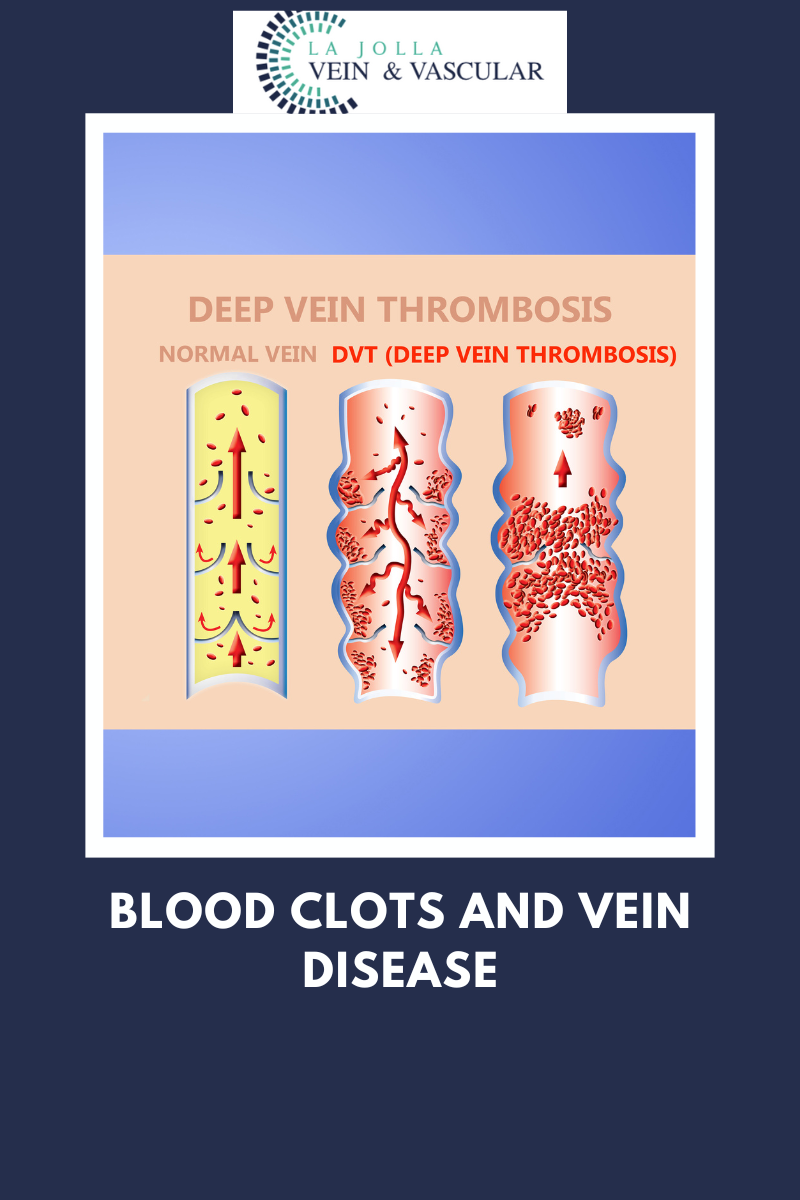
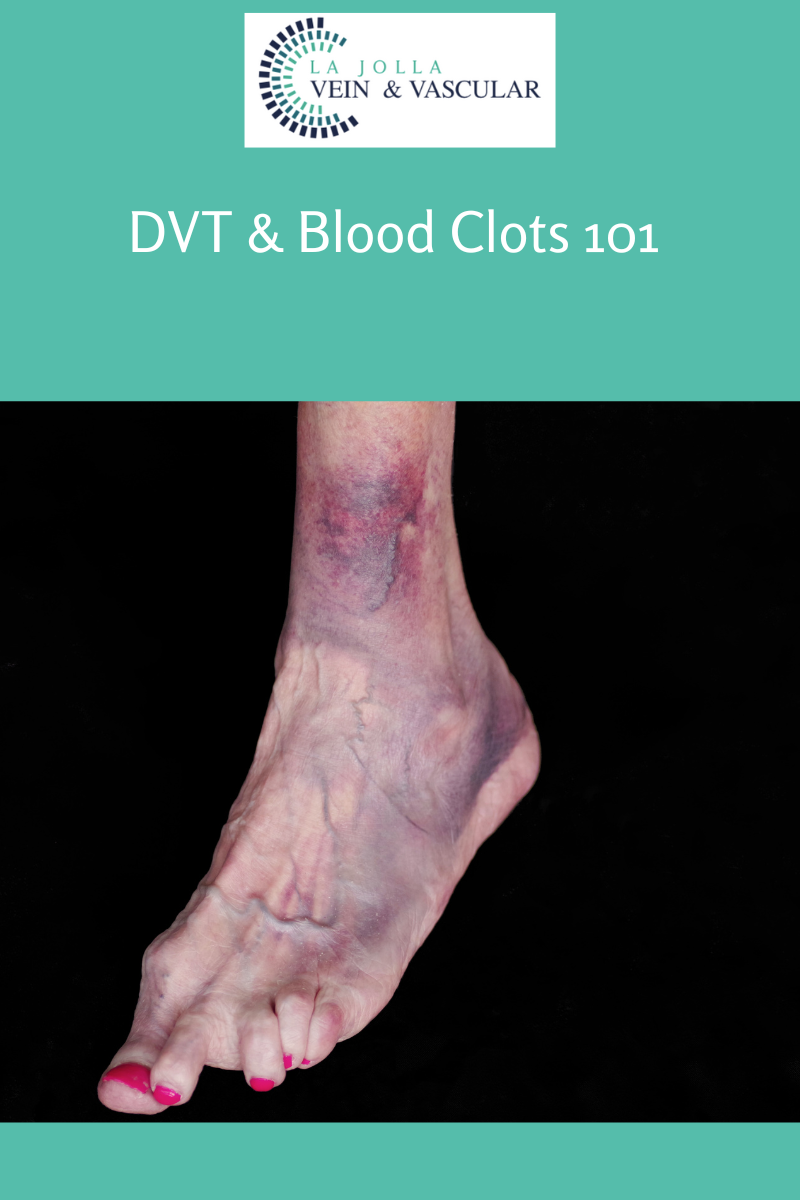
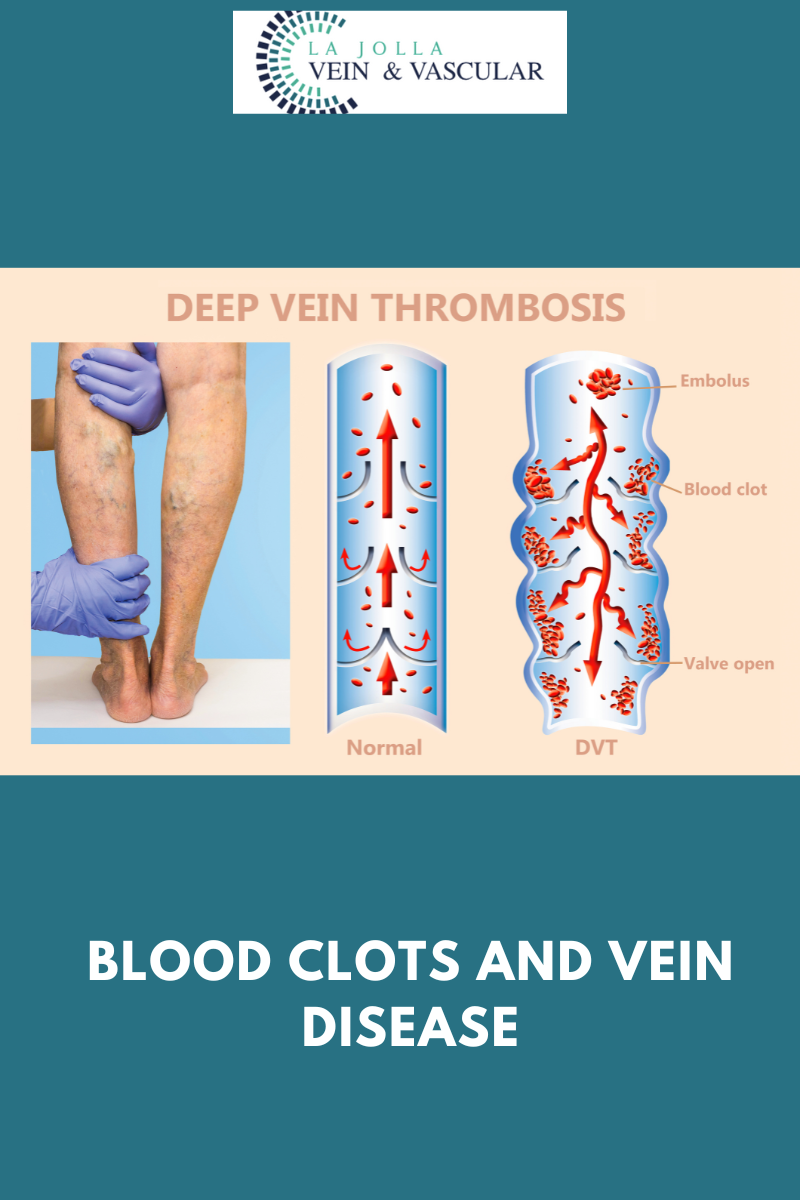
LJVascular2025-09-04T12:19:00-07:00Deep vein thrombosis (DVT) is a serious condition characterized by the formation of blood clots in deep veins, most commonly in the legs. Often, individuals may not experience any symptoms, but when they do manifest, recognizing them promptly is crucial for seeking medical attention and preventing complications. Let’s explore the signs and symptoms […]