Exploring upper extremity venous study: insights
LJVascular2024-10-24T19:40:28-07:00Exploring upper extremity venous study: insights
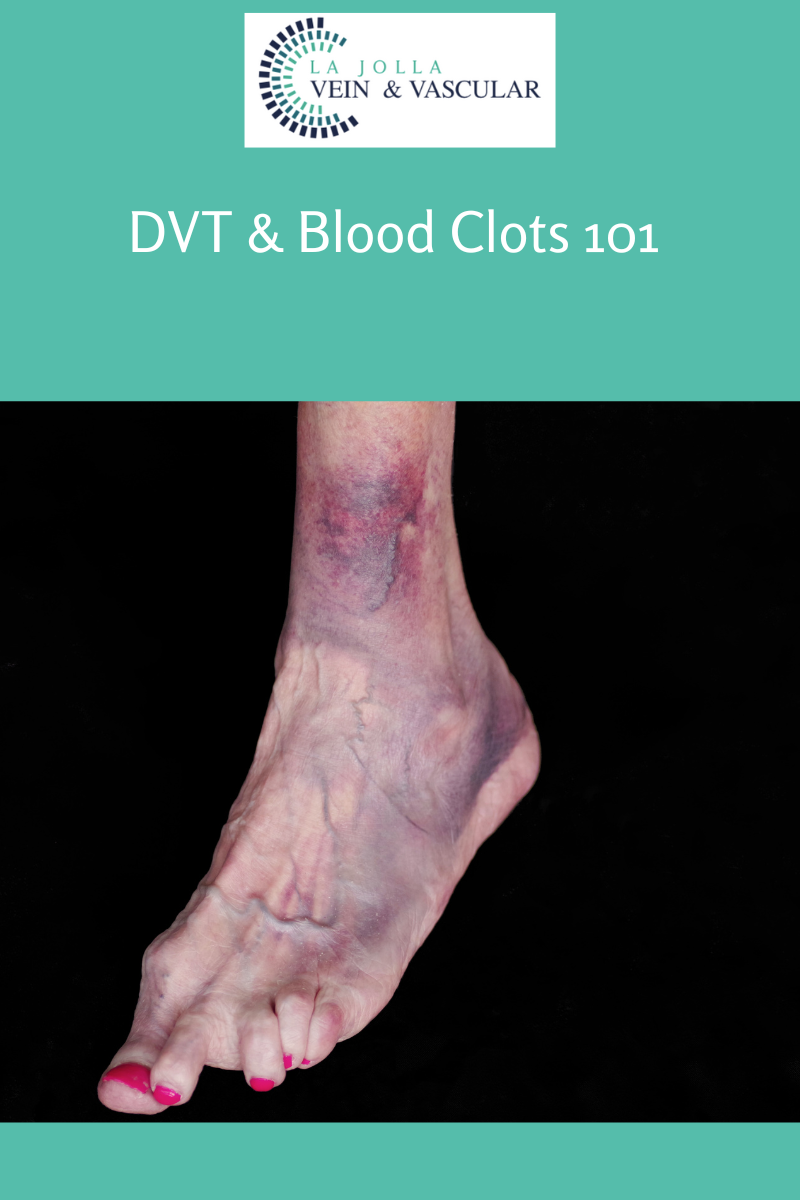
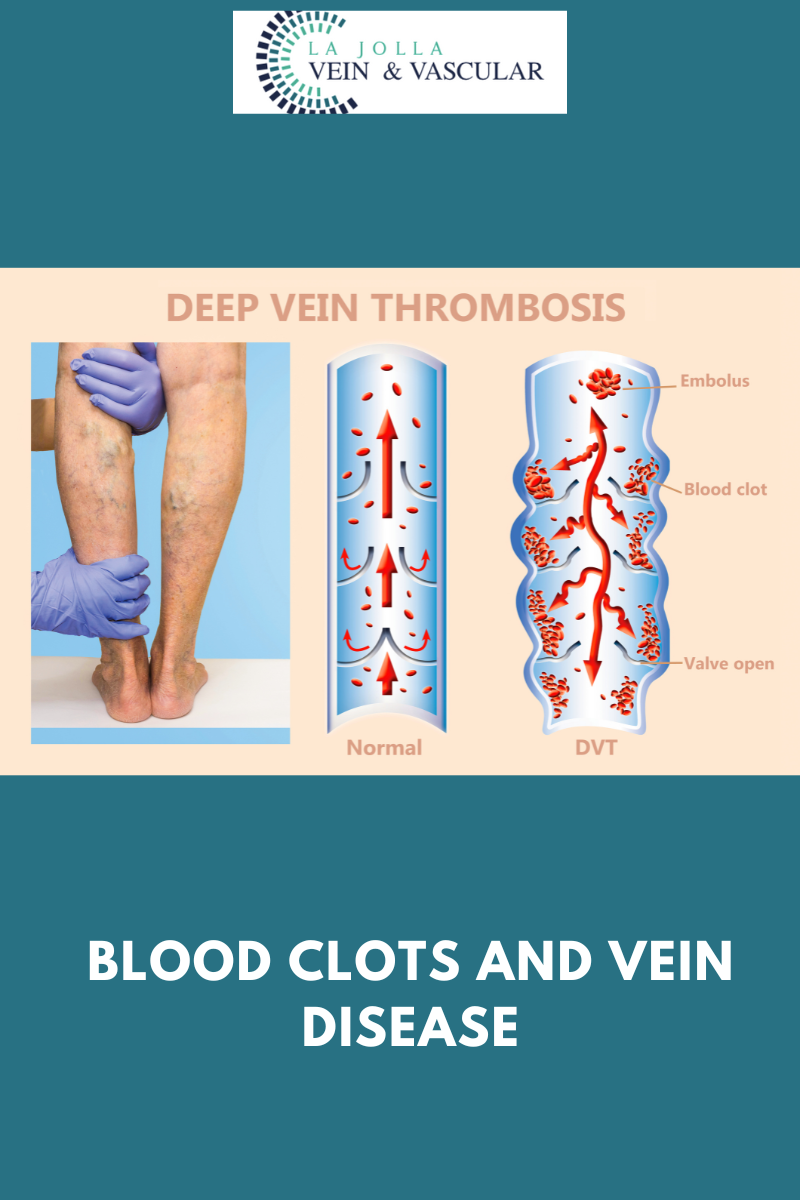
While deep vein thrombosis (DVT) in the legs often takes the spotlight, it’s essential not to overlook the upper extremities when assessing vein health. An Upper Extremity Venous Study, a specialized ultrasound examination, plays a pivotal role in uncovering potential issues in the arms and […]