Will my skin change with chronic venous insufficiency?
LJVascular2024-06-09T11:09:17-07:00Within the sphere of vascular health, Chronic Venous Insufficiency (CVI) stands as a prevalent yet often misconstrued condition. Characterized by a cascade of symptoms that can ultimately result in skin changes and ulcers, CVI necessitates attention and effective management. In this article, we’ll navigate through the intricacies of CVI, shedding light on its symptoms, causes, and, significantly, its treatment.
Unraveling Chronic Venous Insufficiency

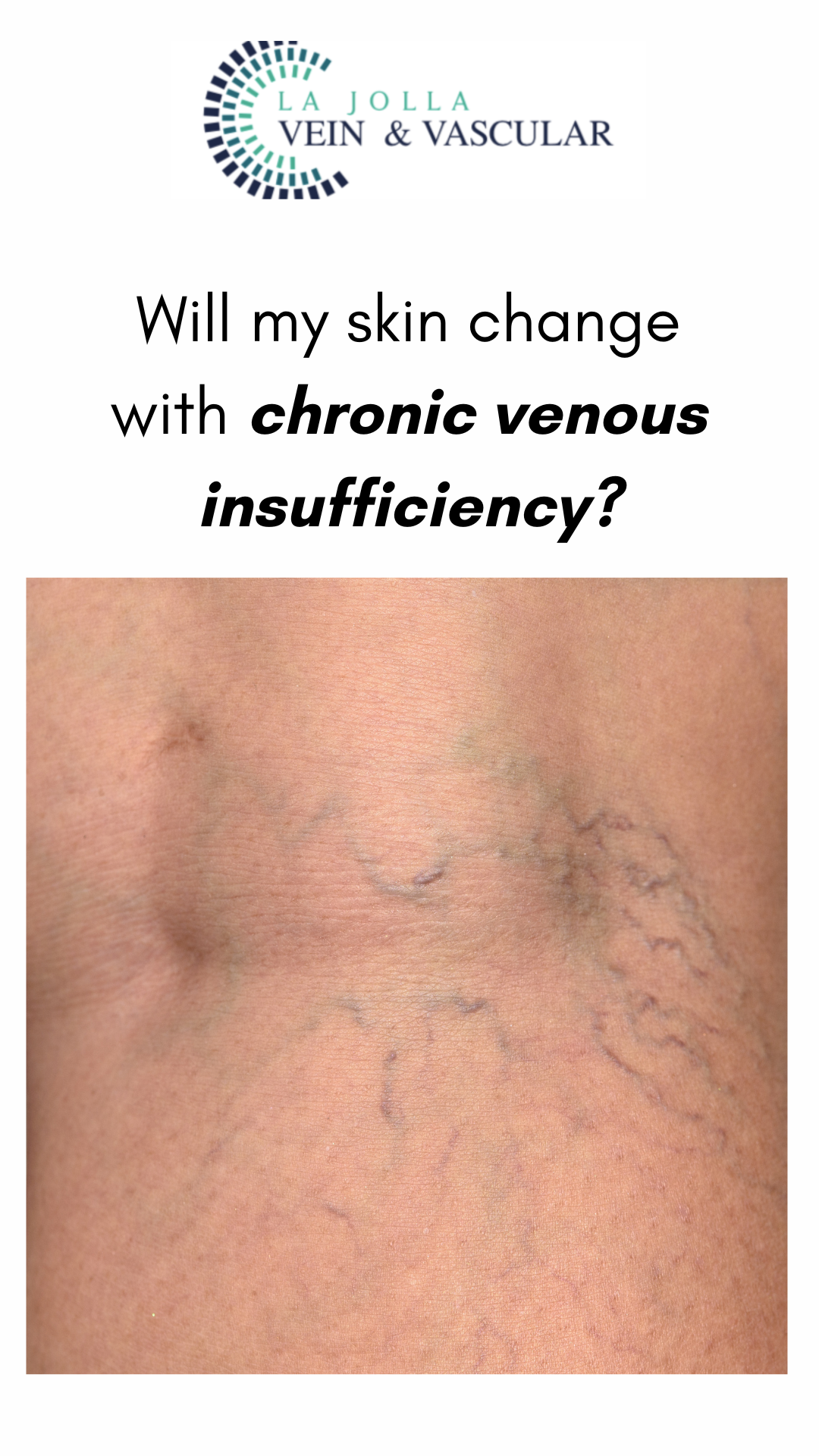
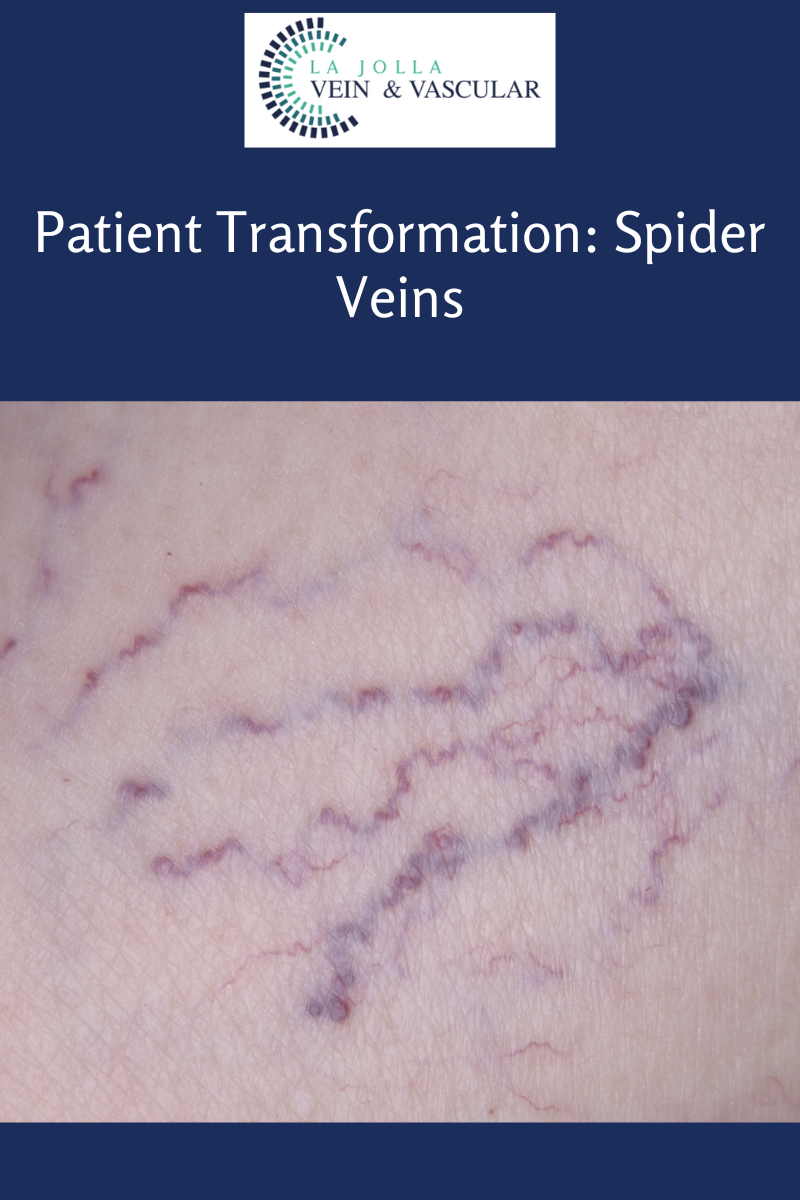
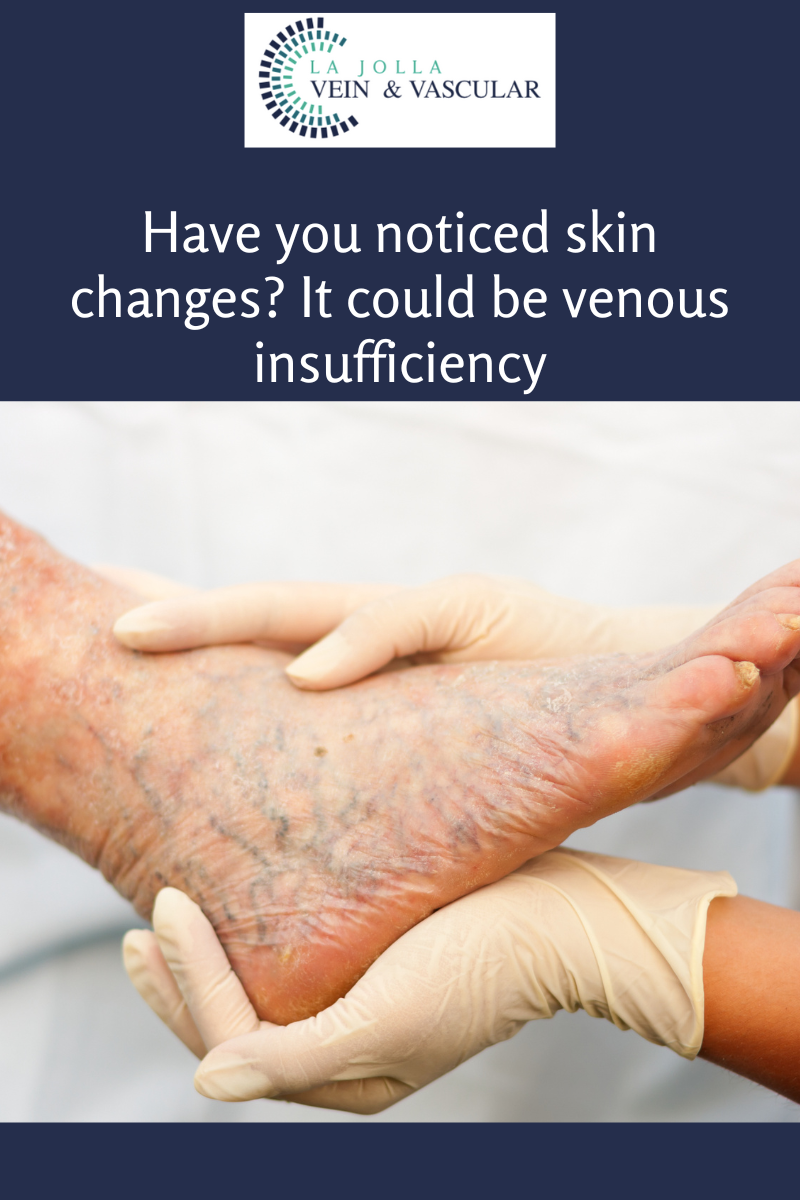
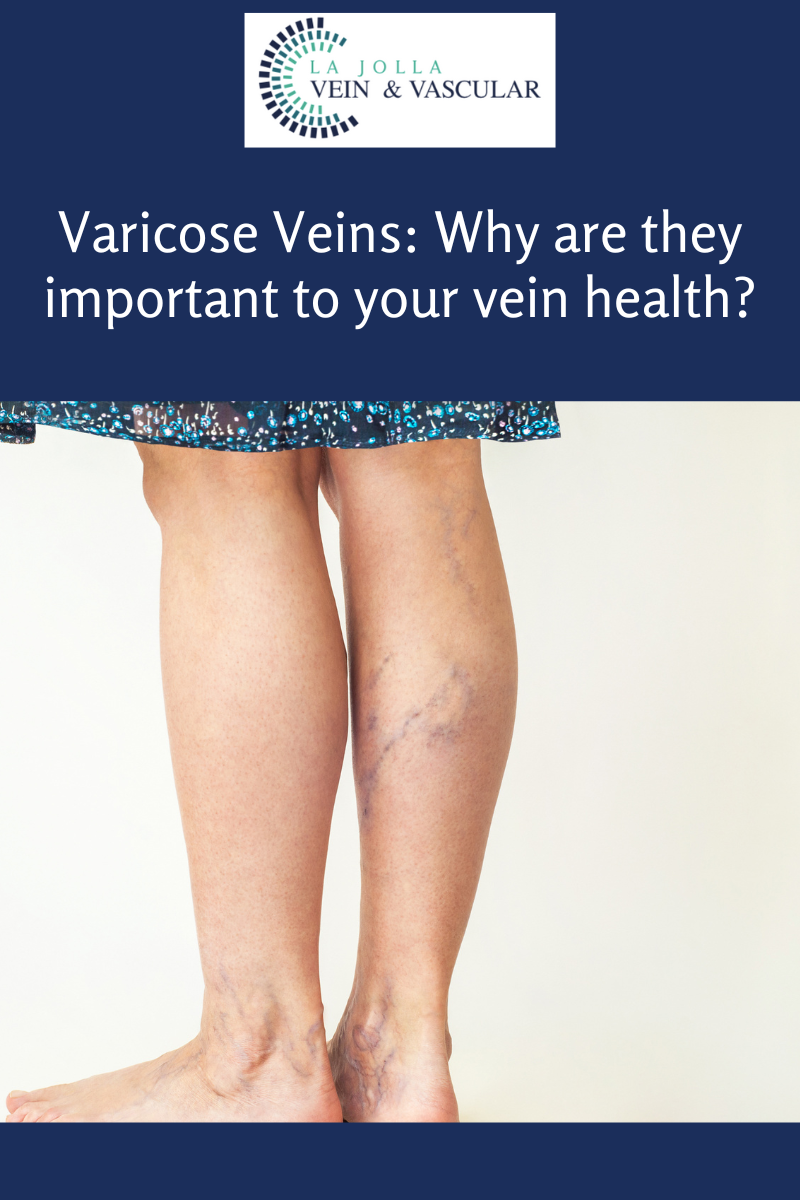
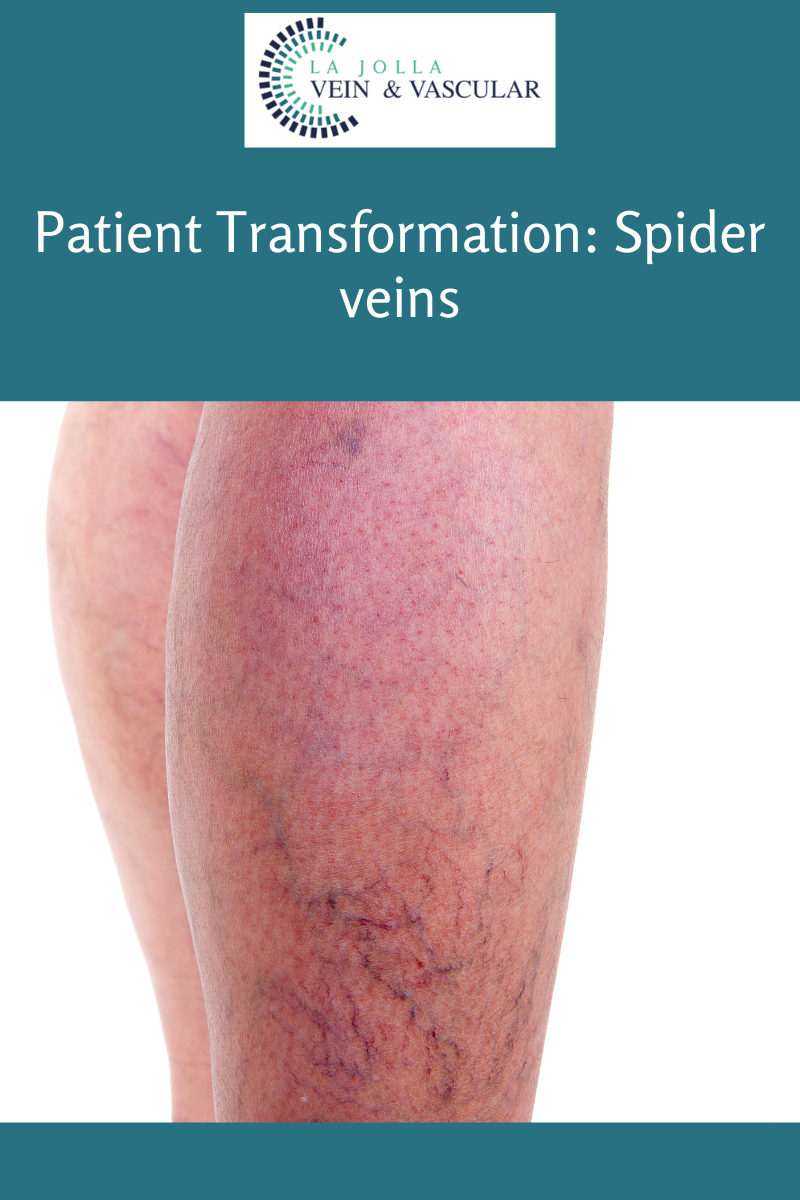
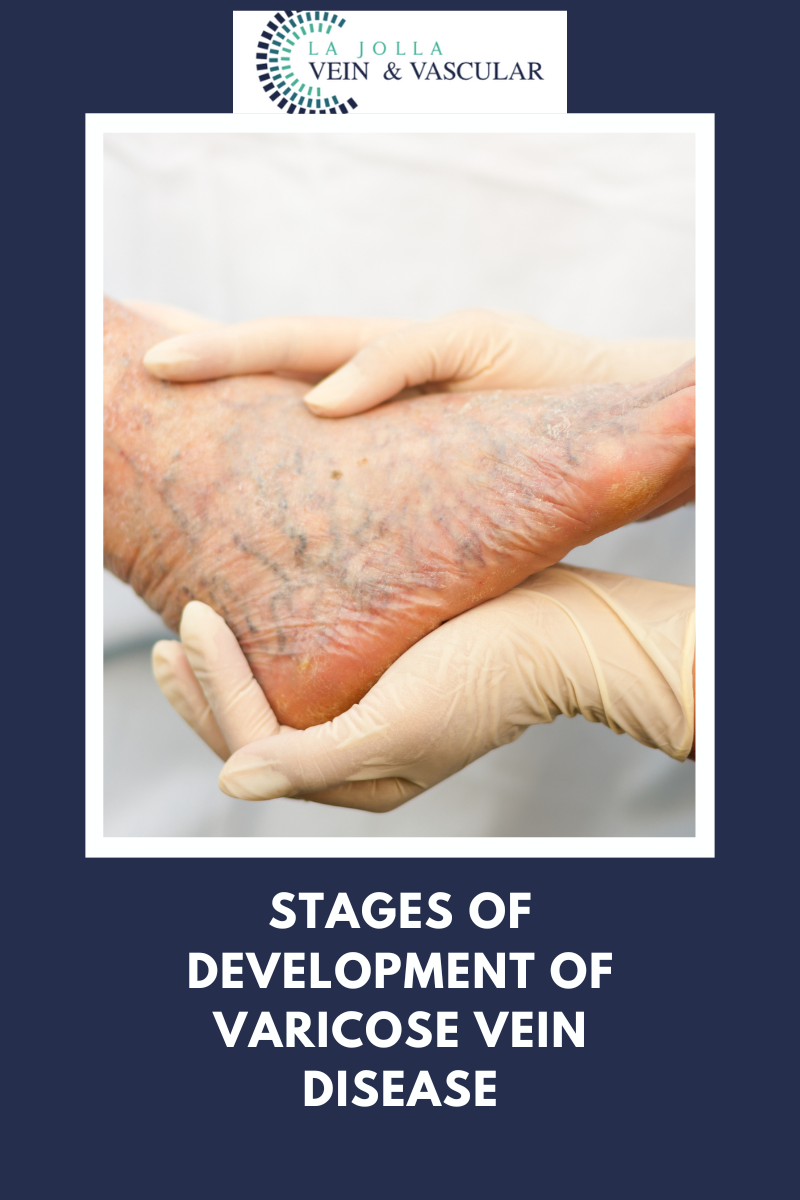
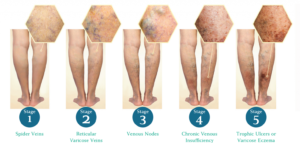
Chronic venous insufficiency arises from a complex interplay of factors, primarily rooted in untreated venous reflux disease. Initial signs encompass discomforts like leg swelling, fatigue, and varicose veins, yet the condition can progressively worsen. As blood circulation falters within the leg veins, the skin undergoes changes marking the onset of chronic venous insufficiency. These changes, referred to as venous stasis, encapsulate the skin’s darkening, dryness, itchiness, and firmness. In severe cases, this deterioration can lead to skin breakdown and ulceration, known as venous leg ulcers or stasis ulcers.
Symptoms and Skin Changes of CVI
The symptoms of CVI extend beyond physical discomfort, manifesting in visible alterations in the skin. Venous stasis skin changes linked with chronic venous insufficiency comprise:
Darkened Skin along the Ankles: Disrupted blood flow leads to a darker hue, particularly around the ankles.
Itching and Dryness around the Ankles (Venous Eczema): Persistent irritation and dryness result in continuous itching and discomfort.
Formation of Wounds around the Ankles: Termed venous leg ulcers, these non-healing wounds necessitate specific attention and care.
Taking Control: Treating CVI
While the skin changes induced by CVI may be irreversible, managing the condition is crucial to impede its progression and prevent ulcers. Addressing the underlying venous reflux constitutes a pivotal aspect of managing CVI. By doing so, inflammatory changes may diminish, potentially improving skin symptoms. However, it’s essential to note that permanent skin discoloration might persist despite successful reflux treatment.
Treating Venous Leg Ulcers
For individuals progressing to venous leg ulcers, treatment necessitates a multi-faceted approach:
Correcting Underlying Venous Reflux: Addressing the root cause is paramount. Treatment methods vary based on the location of the underlying reflux, determined through a comprehensive ultrasound.
Referral to a Wound Care Clinic: Collaborating with wound care specialists adept at managing venous leg ulcers expedites the healing process through their expertise and treatments.
Compression Therapy: Employing compression garments aids in enhancing blood circulation and fostering healing, serving as a cornerstone in venous ulcer management.
Chronic venous insufficiency is a condition that commands attention, education, and diligent management. Understanding its implications and proper management strategies play crucial roles in averting complications and promoting healing.
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Amanda Steinberger, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!