How to Treat Leg Spider Veins
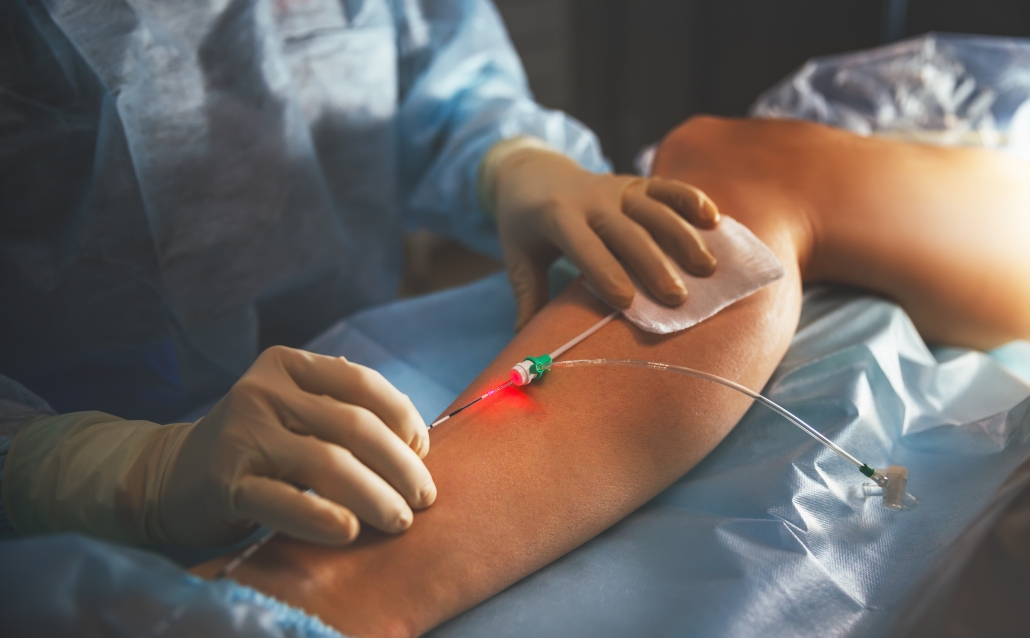
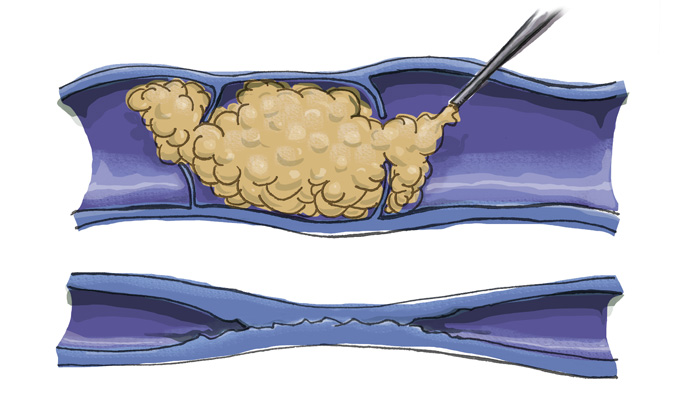
Nisha Bunke2020-09-18T19:01:10-07:00Spider veins and reticular veins of the legs are most commonly treated with sclerotherapy. Sclerotherapy involves an injection of a medication into the vein. This will cause the vein to collapse and gradually fade away. Sclerotherapy has been used to treat spider veins for decades, but modern solutions such as Asclera, allow for spider […]