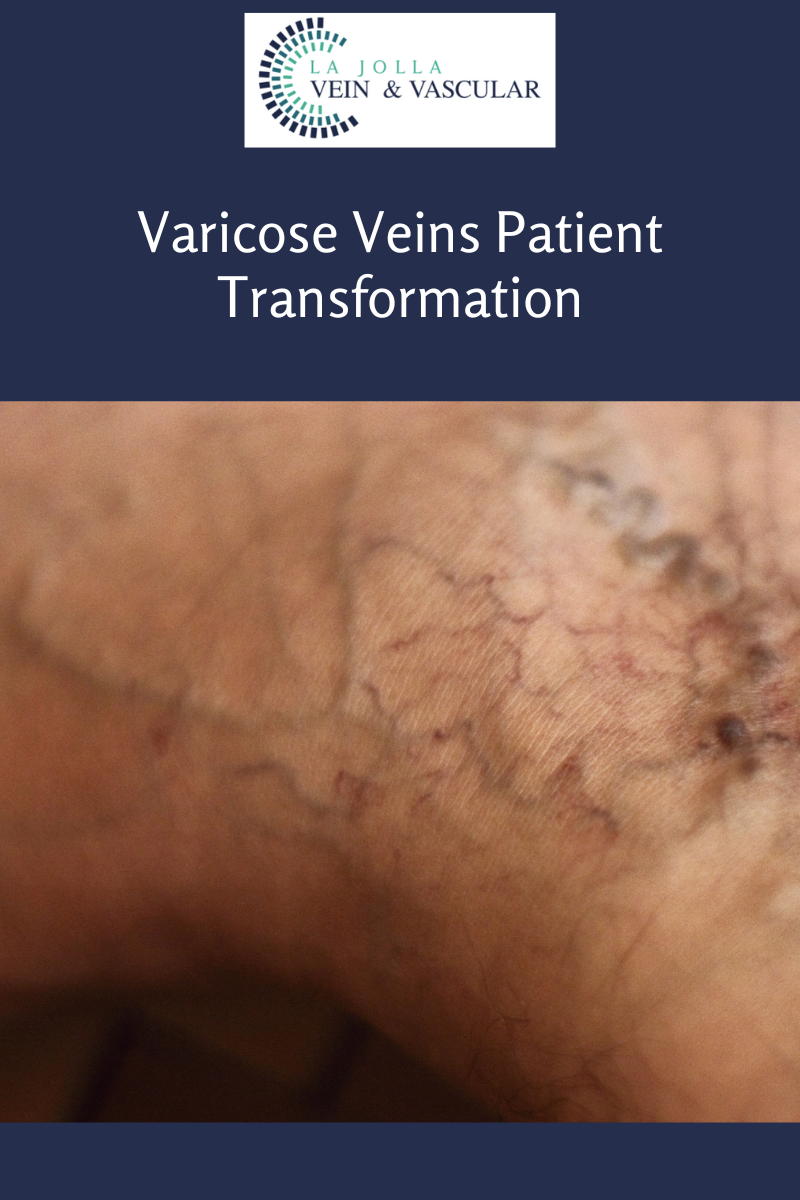
Varicose Veins & Treatment
LJVascular2022-12-26T11:36:19-08:00Endovenous laser vein ablation, also known as endovenous laser therapy (EVLA), is a type of treatment for saphenous vein reflux, the underlying cause of most varicose veins. At La Jolla Vein Care, we offer ALL treatment modalities for varicose veins, not just one. Treatment is customized based on a person’s individual pattern of […]