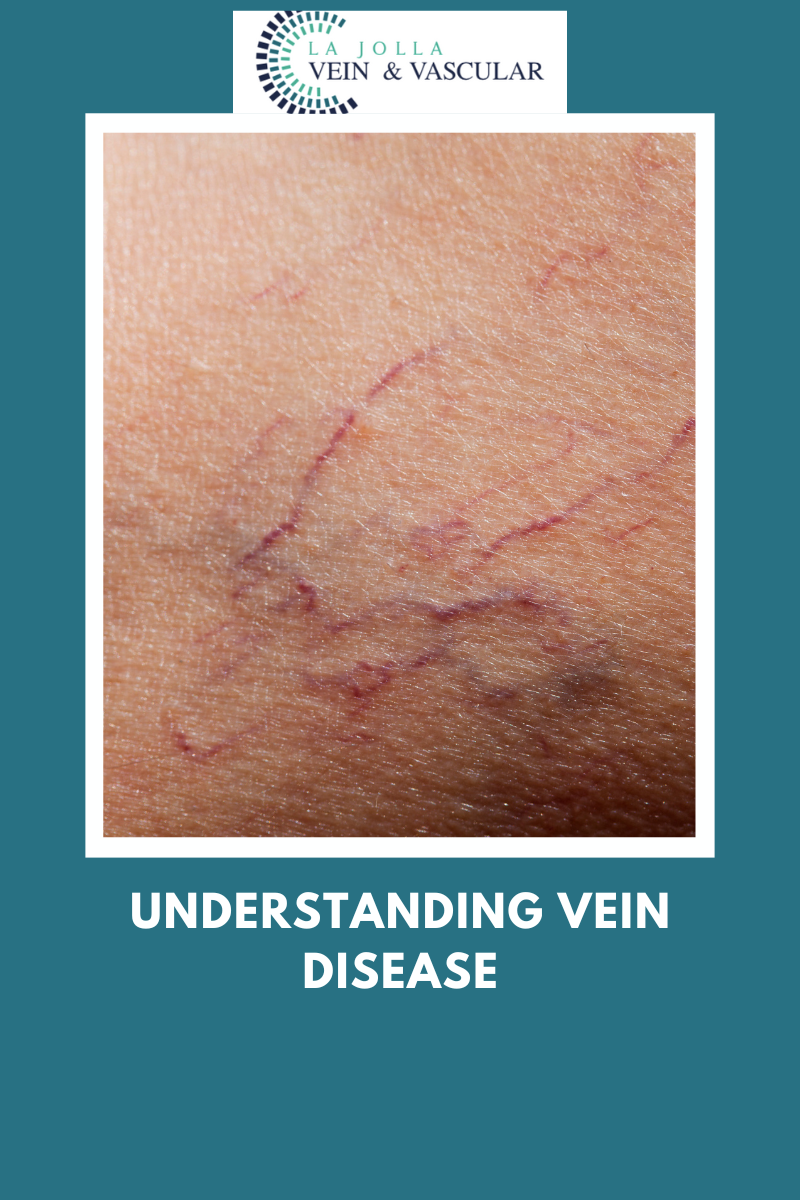
Understanding Vein Disease
LJVascular2023-01-14T13:09:15-08:00What is Venous Reflux Disease?
Venous reflux disease of the veins is also known as venous stasis, venous insufficiency or venous incompetence. Venous reflux disease refers to ‘leaky valves’ in the legs.
Reflux may occur in the deep and/or superficial leg veins. Those located in the deep are those within the muscle; they […]