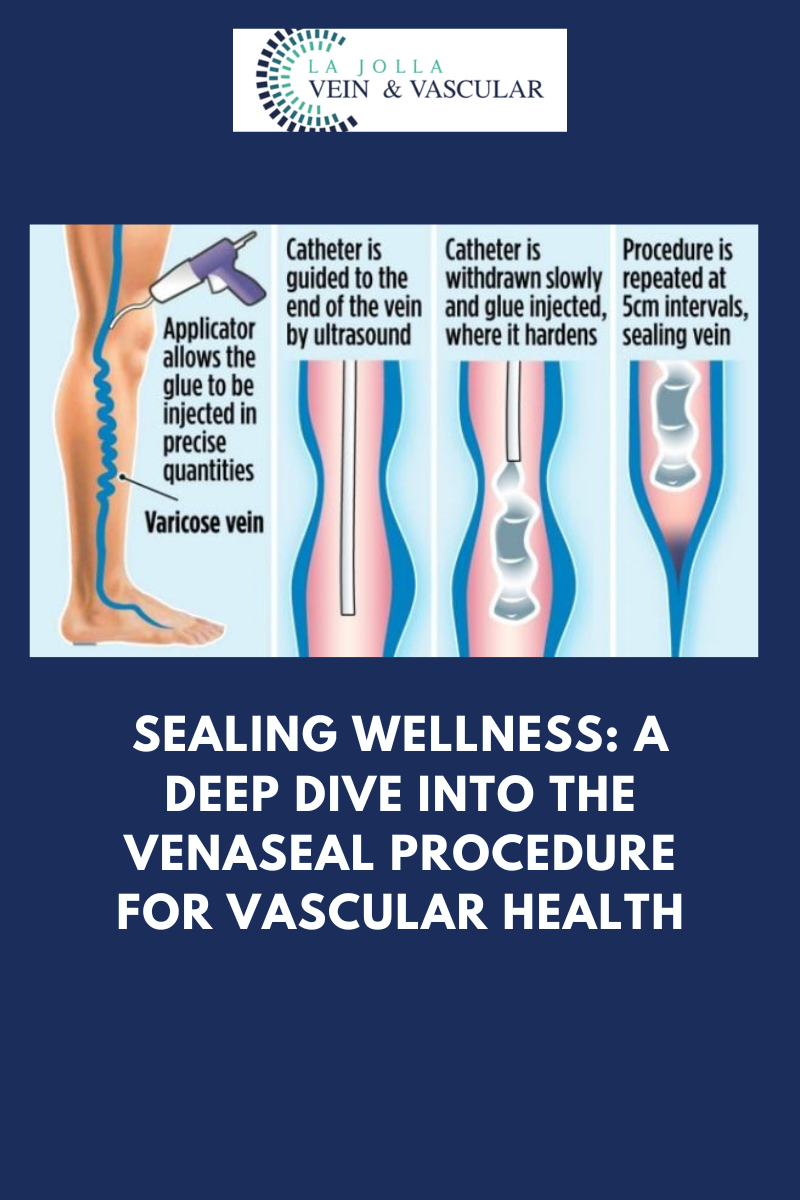
Sealing wellness: A deep dive into the Venaseal procedure for vascular health
LJVascular2024-10-28T07:23:18-07:00Sealing Wellness: A Deep Dive into the Venaseal Procedure for Vascular Health
The VenaSeal™ closure system, approved by the U.S. Food and Drug Administration (FDA), offers an innovative and effective way to treat varicose veins. Unlike traditional methods, this minimally invasive procedure utilizes a unique medical adhesive to permanently seal affected superficial […]