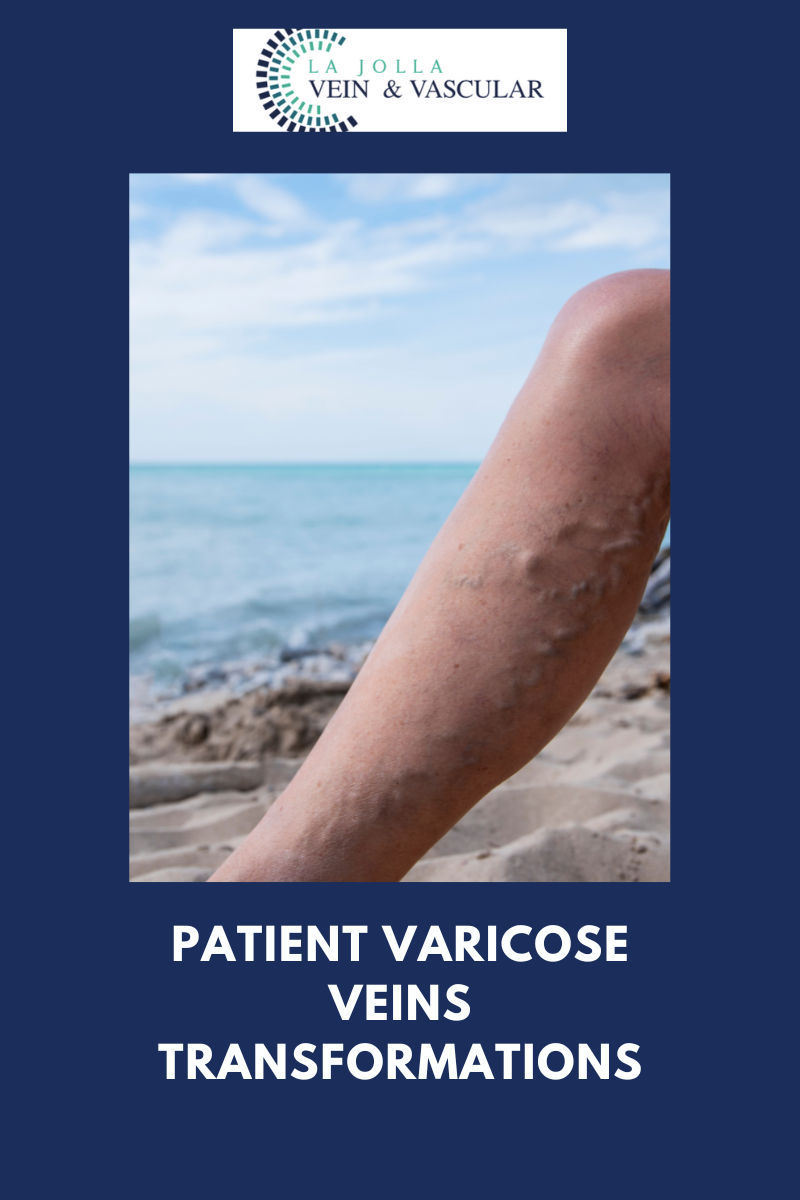
Patient varicose veins transformations
LJVascular2024-10-31T21:20:52-07:00Patient Varicose Veins Transformations
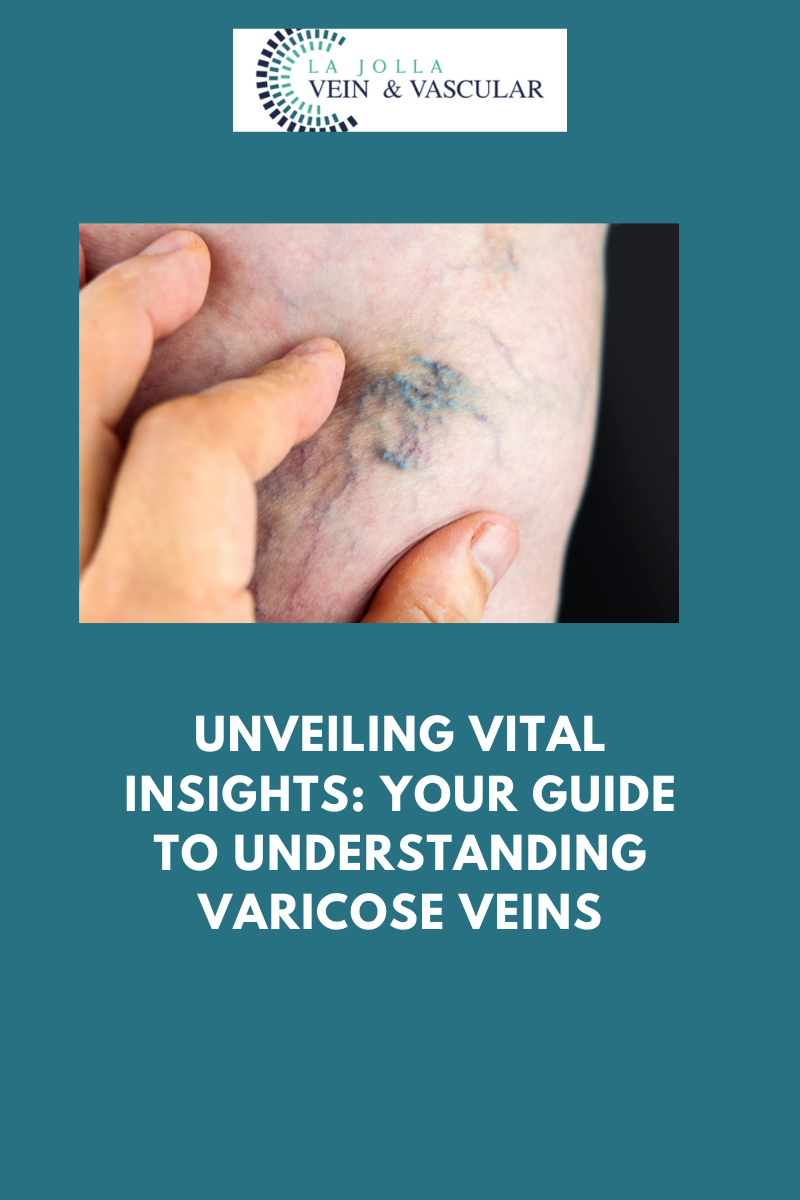
Varicose veins, those twisted and bulging veins just beneath the surface of the skin, can be a common concern for many individuals. While they most frequently appear in the legs, they can also emerge in other areas of the body. In this blog post, we’ll delve into the world of […]