8 Warning Signs of Vein Disease: #2 Discoloration of the Skin
La Jolla Vein Care2021-11-03T17:41:45-07:00Discoloration of the Skin
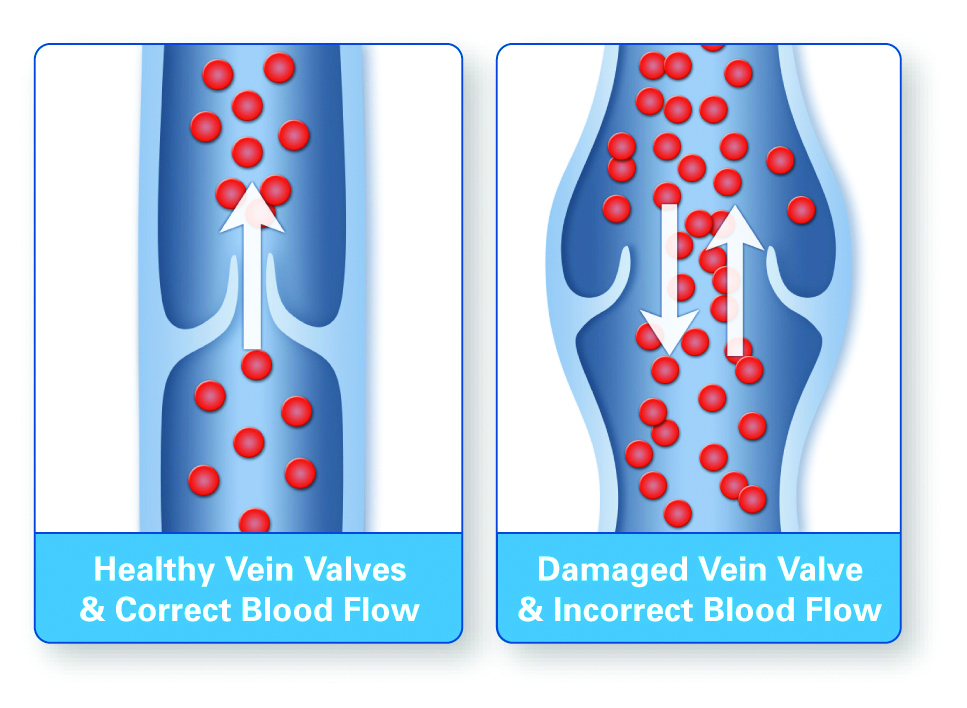
Over time, leakage of the blood into the area surrounding the veins can cause tissue to die. The resulting pooling of blood in the tissue causes a darkening of the skin. It is at this stage that the skin is actually stained by your own blood. This is also known as […]