7, 5, 2020
Varicose Veins Common Cause For Restless Legs Symptoms
Nisha Bunke2021-11-15T13:32:16-08:00The restless leg was a reported symptom in 30% of people who suffer from varicose veins, in our study.

Those who suffer from varicose veins often report a feeling of restless legs, especially at night when in bed. In our study, about 30% of […]
Varicose Veins are Inherited
Nisha Bunke2020-08-19T01:12:15-07:00This picture shows the strong correlation between genetics and varicose veins.
One of the strongest risk factors for varicose veins is a family history. We often see mothers and their daughters, fathers and sons, siblings, and some times the entire family for similar varicose vein issues. This picture demonstrates a mother and her daughter with ironically […]
27, 4, 2020
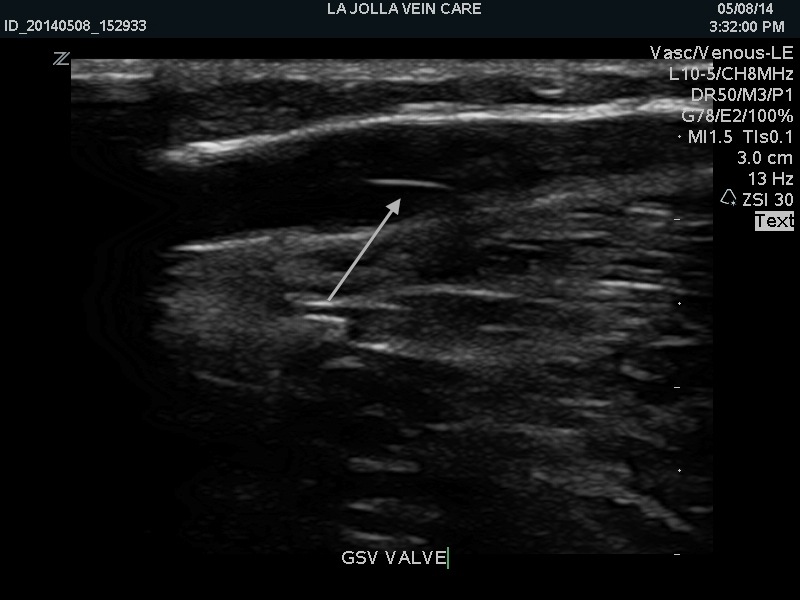
Vein Valves Don’t Work in Venous Reflux Disease
Nisha Bunke2021-11-15T13:17:51-08:00Vein valves and the direction of blood flow can be seen on ultrasound. Ultrasound is an important tool in the diagnosis of venous reflux disease.

In the circulatory system, the veins carry de-oxygenated blood back to the heart. The leg […]
Warm Weather Worsens Leg Symptoms
Nisha Bunke2020-08-19T01:00:26-07:00Warm weather can worsen symptoms of varicose veins and venous reflux disease.
This weekend, most of San Diego was blessed with sunny, warm-weather. Warmer weather tends to worsen symptoms of varicose veins, like increased leg heaviness, pain or you may feel that your legs fatigue more quickly during warm weather. For those who have spider veins, […]
Study Finds Nearly 50% Nurses Have Venous Reflux
Nisha Bunke2022-01-04T10:10:57-08:00Women in nursing professions are at high risk for developing varicose veins as it requires physical work and prolonged standing.
It is well known to vein specialists that individuals with occupations that require long periods of standing such as nurses, physicians, other health care workers, retail workers, flight attendants, hairdressers, etc. have a higher incidence of
Night Cramps Commonly Caused by Varicose Veins
Nisha Bunke2021-12-31T12:29:50-08:00Leg cramps occurring at night (nocturnal leg cramps) are a common symptom of venous disease. In fact, in the San Diego Population Study, leg cramps were the second most common symptom in people with the venous disease with a prevalence of 14.3%. Leg aching (17.7%) was the most common complaint and tired and […]
Health Risks of Working-From-Home
Nisha Bunke2020-08-19T00:48:02-07:00Prolonged desk work can increase the risk of blood clots in leg veins.
As many Americans are working from home, we have received many calls from patients regarding thrombophlebitis. This is not a new scenario for us, over the years frequently patients come in for assessment of leg pain after working on their computers for 12 […]
Wendy Williams Show Kathy Bates Bring Light to Lymphedema
Nisha Bunke2021-11-15T11:03:12-08:00Both Wendy Williams and Kathy Bates Suffer from Lymphedema.
This week’s Wendy Williams Show host, Wendy Williams discussed her struggles with lymphedema with guest, Kathy Bates who also has lymphedema. They both agreed that lymphedema is not given enough attention in medical education and in the medical community. We agree. Our medical speciality and society […]
Olympic Athletes Who Suffer from Varicose Veins
Nisha Bunke2022-01-03T13:04:37-08:00Even Olympic gold medalists get varicose veins! Including swimmers and beach volleyball players…….
It is a huge misconception that people who take care of their bodies don’t get varicose veins. In contrast, most of our patients take great care of their health. At La Jolla Vein Care, we routinely care for competitive athletes, marathon runners, […]