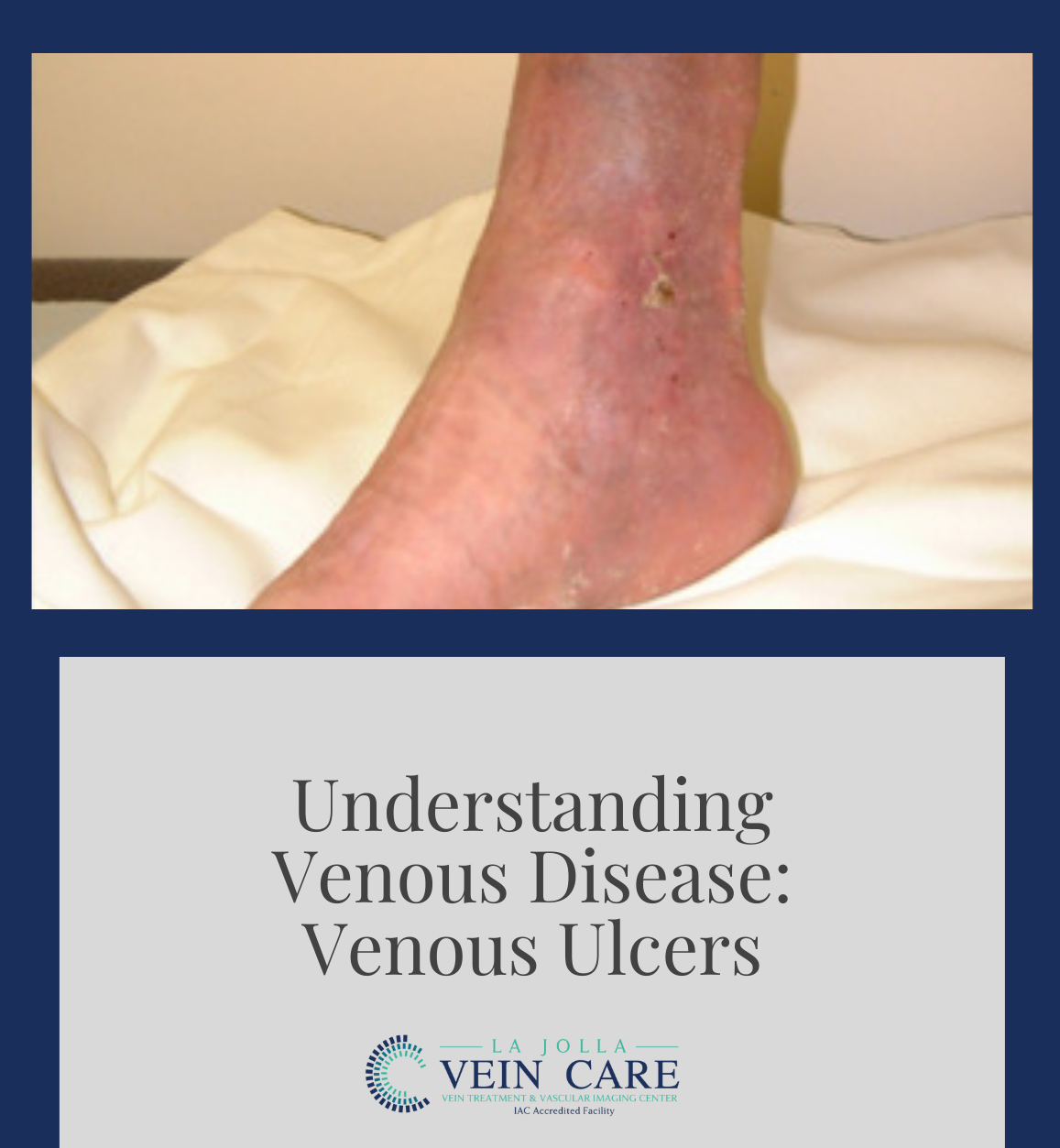
Understanding Venous Disease: Venous Ulcers
LJVascular2022-04-23T14:20:59-07:00Understanding Venous Disease: Venous Ulcers
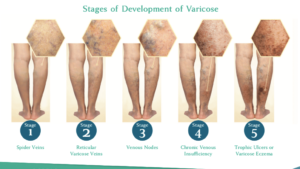
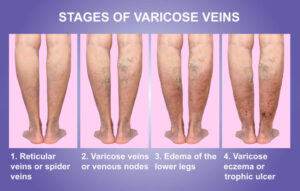
A venous leg ulcer is the most severe form of chronic venous insufficiency. This is referred to as a ‘venous leg ulcer.’ Venous ulcers of the leg make up 70% of all chronic leg wounds. Therefore, a venous leg ulcer is much more common than a diabetic or arterial […]