Varicose veins can appear in the pelvis
LJVascular2023-05-24T18:38:46-07:00PVC: Most people know varicose veins mostly affect the feet and legs. But varicose veins can also occur in the pelvis causing chronic pelvic pain in women; this condition is known as Pelvic Venous Congestion Syndrome (PVCs) or ovarian vein reflux. Herein is a look at the condition, the risk factors, causes, symptoms, and treatment options. Read on to find out more.
What is pelvic venous congestion syndrome (PVCs)?
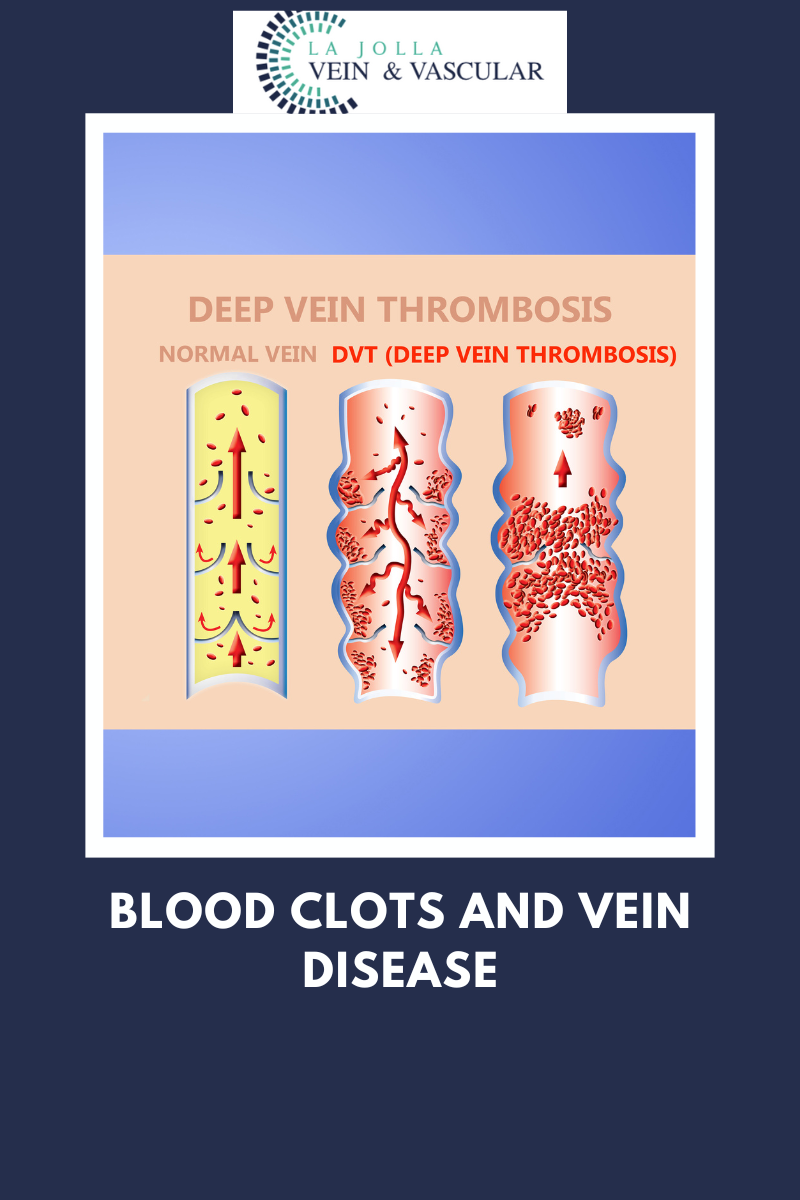
Pelvic Venous congestion is the enlargement of blood vessels in the pelvis due to faulty vein valves in the lower abdomen. See, veins have valves to guide blood flow towards the heart. However, these valves become faulty in some cases due to damage or other problems causing blood to flow backward. When this happens in the lower abdomen, blood builds up in the area, causing the veins to enlarge and change shape.
Therefore, PVCs are varicose veins in your pelvis. This engorgement or congestion of blood vessels in the lower abdomen can cause chronic, unbearable pain. It affects at least 1 in three women at some point during their lifetime. Chronic PVCs last more than six months. It is not associated with period pain at all. PVCs are common among women who’ve given birth more than once.
Symptoms to Look Out For
Chronic PVCs last longer than half a year. PVCs are commonly experienced for the first time during or following pregnancy. It is characterized by a heavy aching feeling that may get worse as pregnancy progresses. In most cases, you feel the pain on the left side only. But at other times, you may feel the pain on both the left and right sides. PVCs pain is usually worse during the evenings.
Certain factors also aggravate PVCs pain; these include:
- When you change posture
- Sex
- Standing for extended periods
- Walking
- Menstrual period
Apart from pelvis pain, other PVCs symptoms include:
- Pain during or after intercourse
- Sudden urge to urinate
- Lower back pain
- Irritable bowel syndrome (diarrhea and constant abdominal pain accompanied with constipation)
- Deep dyspareunia – pain during intercourse
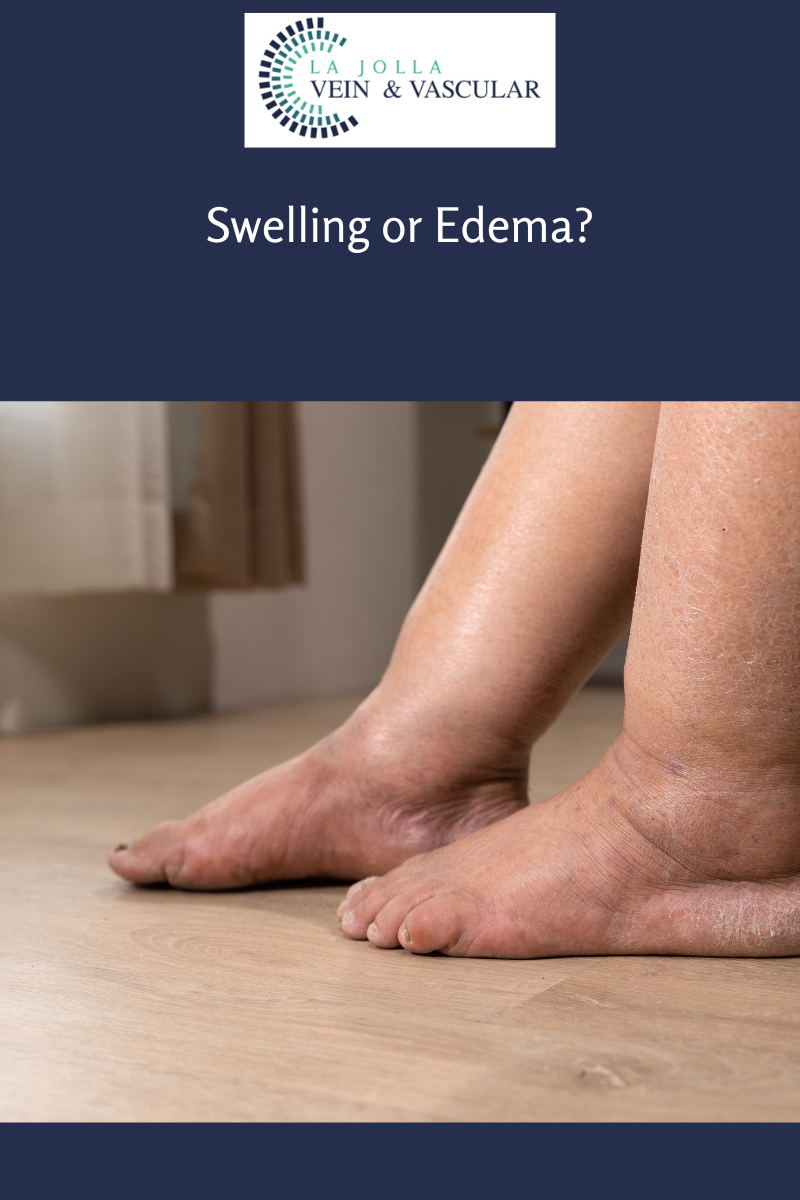
- Feeling one’s legs fuller
- Engorged and distorted veins around the vagina, vulva, inner thigh, buttocks, and sometimes down the legs
“Bringing Experts Together for Unparalleled Vein and Vascular Care”
La Jolla Vein & Vascular (formerly La Jolla Vein Care) is committed to bringing experts together for unparalleled vein and vascular care.
Nisha Bunke, MD, Sarah Lucas, MD, and Elliot DeYoung, MD are specialists who combine their experience and expertise to offer world-class vascular care.
Our accredited center is also a nationally known teaching site and center of excellence.
For more information on treatments and to book a consultation, please give our office a call at 858-550-0330.
For a deeper dive into vein and vascular care, please check out our Youtube Channel at this link, and our website https://ljvascular.com
For more information on varicose veins and eliminating underlying venous insufficiency,
Please follow our social media Instagram Profile and Tik Tok Profile for more fun videos and educational information.
For more blogs and educational content, please check out our clinic’s blog posts!