3-Stage Approach to Vein Treatment
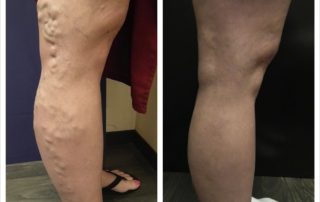
When visible signs of venous disease such as spider veins, varicose veins, or skin changes are present, this is usually the tip of the iceberg, and an underlying vein problem is present. An underlying vein condition (venous reflux disease) can be detected with ultrasound. A treatment plan is focused on treating the underlying vein problems […]