COVID Vaccine Concerns and Blood Clots
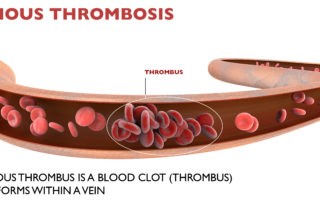
Johnson & Johnson Vaccine Blood Clot Concerns: What is a Deep Vein Thrombosis (DVT)?
Blood clots associated with the Johnson & Johnson vaccine have caused pause and concern. As a result, the United States is recommending a pause on administering the single-dose Johnson & Johnson coronavirus (COVID-19) vaccine after reports of six women experiencing blood clots […]