What is Radiofrequency Treatment for Varicose Veins?
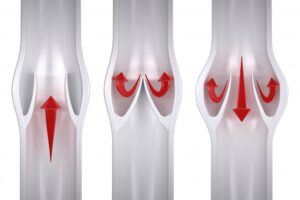
At La Jolla Vein Care, we use a special procedure called radiofrequency treatment for varicose veins. This treatment uses a radiofrequency energy to heat up the wall of the vein. This treatment is used for varicose veins. Varicose veins develop when valves in the veins are damaged and this causes the veins to bulge or twist and stand […]