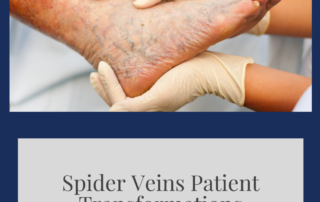
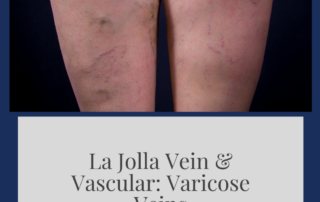
Spider Veins Patient Transformations
What are spider veins?
Spider veins are the fine, thread-like reddish veins at the surface of the skin. Spider veins are not healthy. Spider veins are often considered a cosmetic issue, but they can be associated with underlying feeder veins, not visible to the naked eye. Feeder veins are the ‘blue veins’ […]