Understanding Insurance Coverage for Varicose Veins

Does Insurance Pay for Varicose Vein Treatment? Here are the criteria that determine if insurance pays for varicose vein treatment
Most insurance types (including Medicare and Molina) will cover varicose vein treatments that are considered “medically necessary care” but not for “cosmetic care”. Varicose veins (bulging leg veins) have to cause symptoms such as leg pain to be covered by insurance. Spider veins (tiny clusters of blood vessels at the skins surface) are considered a cosmetic treatment and are not covered by any type of insurance.
4 Main Criteria for medically necessary vein treatment
- Varicose veins must cause leg pain or other symptoms.

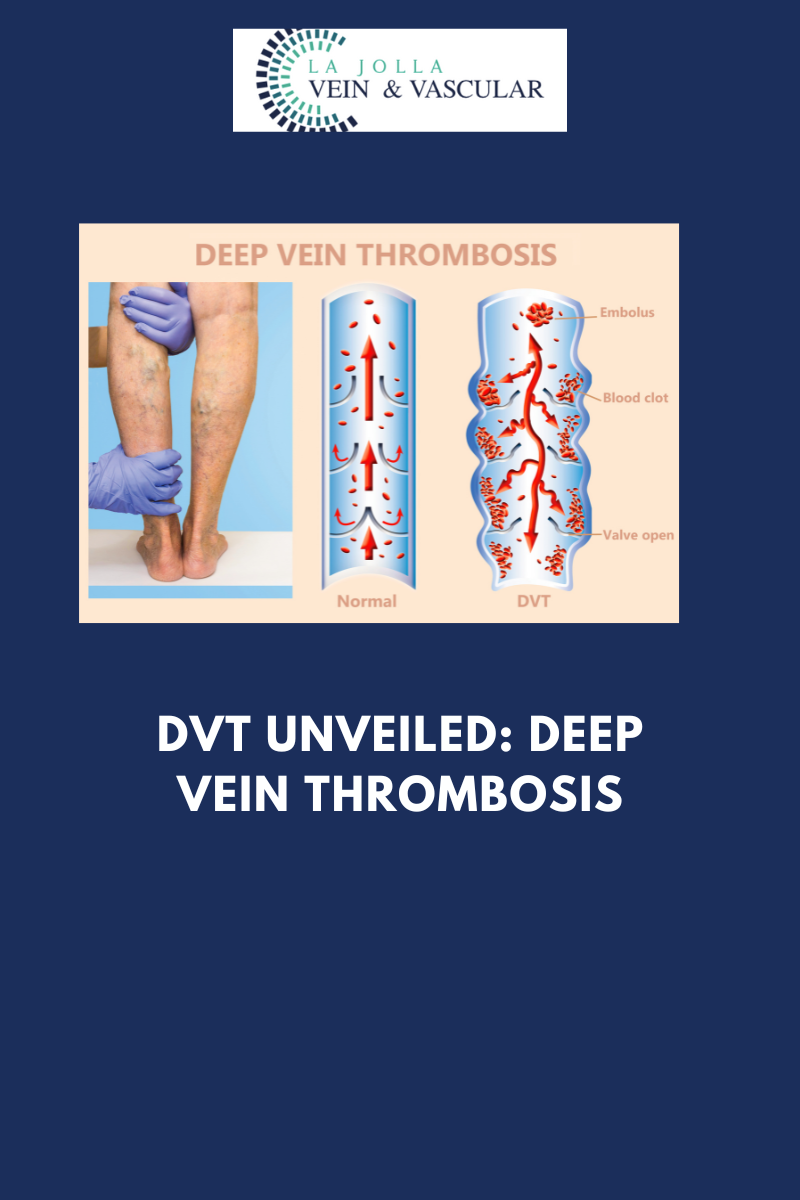
Medically necessary vein treatment means that the varicose veins must cause symptoms such as leg pain, heaviness, persistent swelling, night-time cramping, or burning. Complications of varicose veins that may indicate treatment include leg ulcer (open wound) from the vein problem, recurrent blood clots or phlebitis, ruptured bleeding vein, or skin discoloration around the ankle.
- Symptoms affect daily life.
The symptoms must be severe enough to affect a person’s ability to do their daily routines or work. For example, a teacher may have varicose veins that prevent them from standing and doing their job, because they have to take frequent breaks to elevate their legs. A server at a restaurant may no longer be able to work long shifts, due to leg pain after a few hours. Symptoms can interfere with lifestyle by limiting the amount of exercise one hopes to achieve, or the inability to cook or do house chores due to leg pain.
- Conservative treatment must be tried for 6-12 weeks.
In most cases, insurance requires that conservative measures have been tried for several weeks. Conservative measures include compression stockings, leg elevation, exercise, weight loss, anti-inflammatory medication such as ibuprofen or vasoactive agents such as horse chestnut or Vascular, and hot/cold packs. Many insurance types REQUIRE 6 to 12 weeks of wearing medical-grade compression stockings prior to being approved for treatment. You should have your consultation as soon as possible and begin implementing conservative management into your lifestyle. You should begin keeping a daily log documenting that you are using conservative treatments. If your primary care physician has already prescribed compression stockings, it is helpful if you have a note, you’re your doctor or the prescription, as this counts toward your conservative management time period.
- Venous reflux must be demonstrated on ultrasound.
Underlying venous insufficiency must be documented by ultrasound examination. The ultrasound study to determine the treatment and the physician visits are covered benefits with most insurance types.
Treatments that are not covered by insurance because they are considered to be ‘cosmetic services’ include:
- Varicose veins that do not cause any symptoms
- Spider veins
Does Your Vein Condition Qualify for Medical Necessity?
If you have answered ‘yes’ to each of the 4 categories, then you are likely to meet medical necessity criteria for vein treatment. Disclaimer: this is a simplified questionnaire for patient convenience and understanding.
- Do your varicose veins cause at least one of the following symptoms?
- Leg pain
- Heaviness
- Persistent swelling
- Aching, heaviness, or throbbing
And/ Or have you suffered from one of the following complications of varicose veins?
- Leg ulceration
- Ruptured bleeding vein
- recurrent blood clots or phlebitis
- Do your symptoms (leg pain, etc.) affect your daily life?

- Yes, it affects my job
- Yes, it affects my home
- Yes, it affects my daily routine or leisure
- Have you already tried conservative management and the conservative management has not completely resolved your vein condition?
- Yes, I have tried compression socks/stockings/ AND two or more of the following:
- Leg elevation
- Exercise
- Weight loss
- Ibuprofen or other NSAID
- Ice or heat packs
- Venoactive medication such as Vascular or OTC supplements like horse chestnut or grapeseed extract
- Did you have an ultrasound examination that demonstrated underlying venous reflux disease?
- Yes, my ultrasound demonstrated and documented backward flow in my veins (venous reflux)
- No, the ultrasound examination concluded my veins have normal function.
However, some individual insurance policies exclude varicose vein treatment- this is usually a result of employer exclusion. Sometimes in this case, one may ask the employer to include varicose vein treatments on the policy. You may call the number on the back of your insurance card to ask specifically if they cover vein treatments. When you start a vein treatment process with us, we will help you to understand what your insurance will cover. Our prior authorization specialist will obtain preauthorization (approval) for your treatment and can answer questions.
For a list of insurance types we accept at La Jolla Vein Care, click here.