How is Venous Reflux Diagnosed?
La Jolla Vein Care2021-11-05T11:48:32-07:00
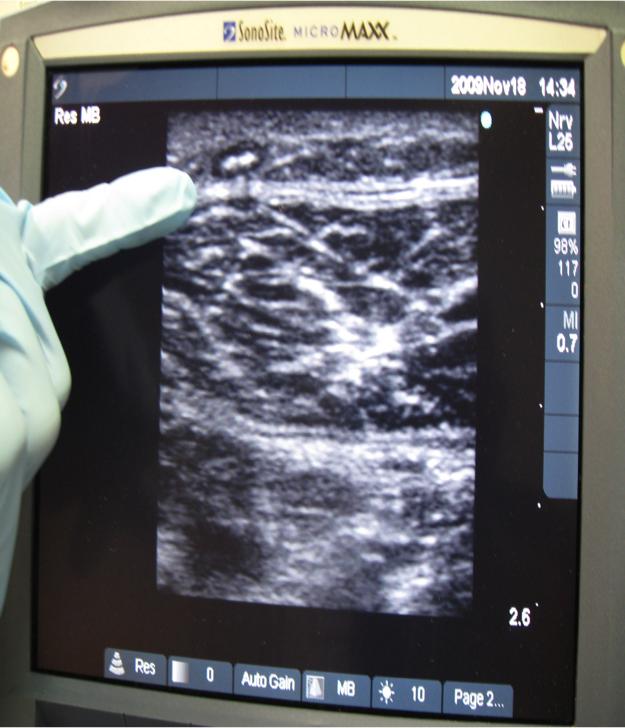
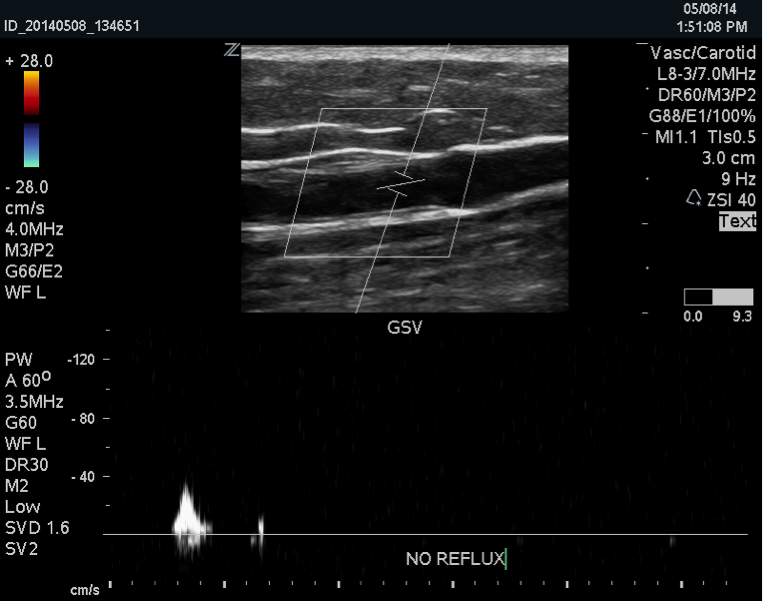
Venous duplex imaging uses ultrasound waves to create pictures. La Jolla Vein Care utilizes state-of-the-art ultrasound scanners to image the veins beneath the surface of the skin, not visible to the naked eye. Duplex ultrasound imaging can identify if the vein is healthy, or if it is refluxing, or if there are any blood clots […]