Easter Dinner & Leg Pain: What’s the Correlation?
Nisha Bunke2021-11-04T19:53:27-07:00After a holiday, patients frequently complain about leg pain. Especially, holidays where hours of cooking are involved like Thanksgiving, Easter, Christmas, Passover, etc. Some people who may have mild venous reflux disease, may not notice any symptoms until they are standing for hours- like during cooking. Over the years, we always hear from patients that […]

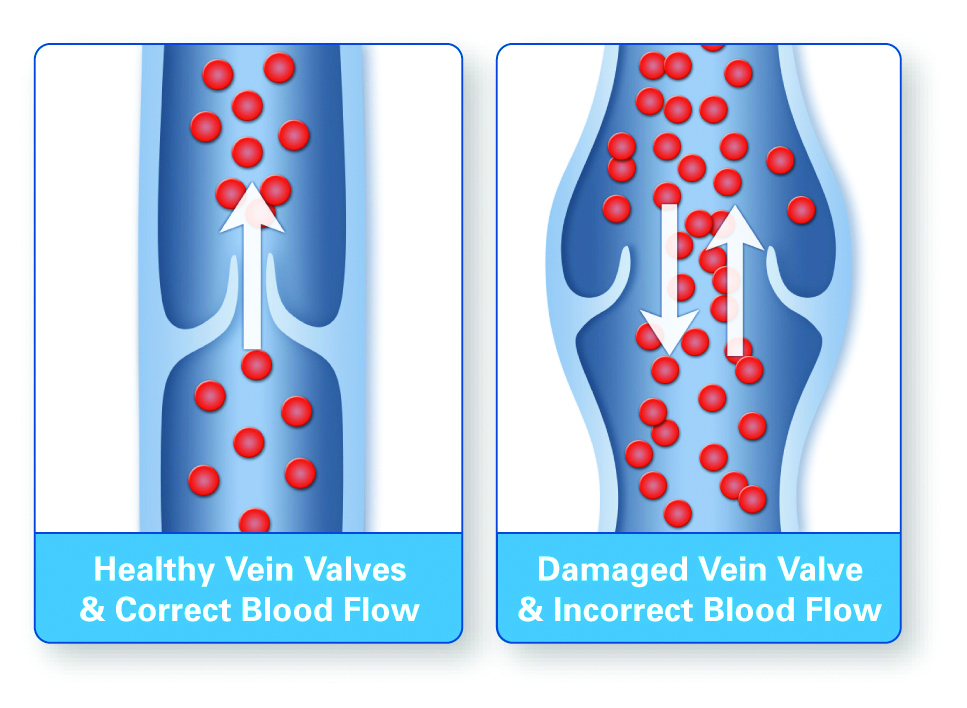
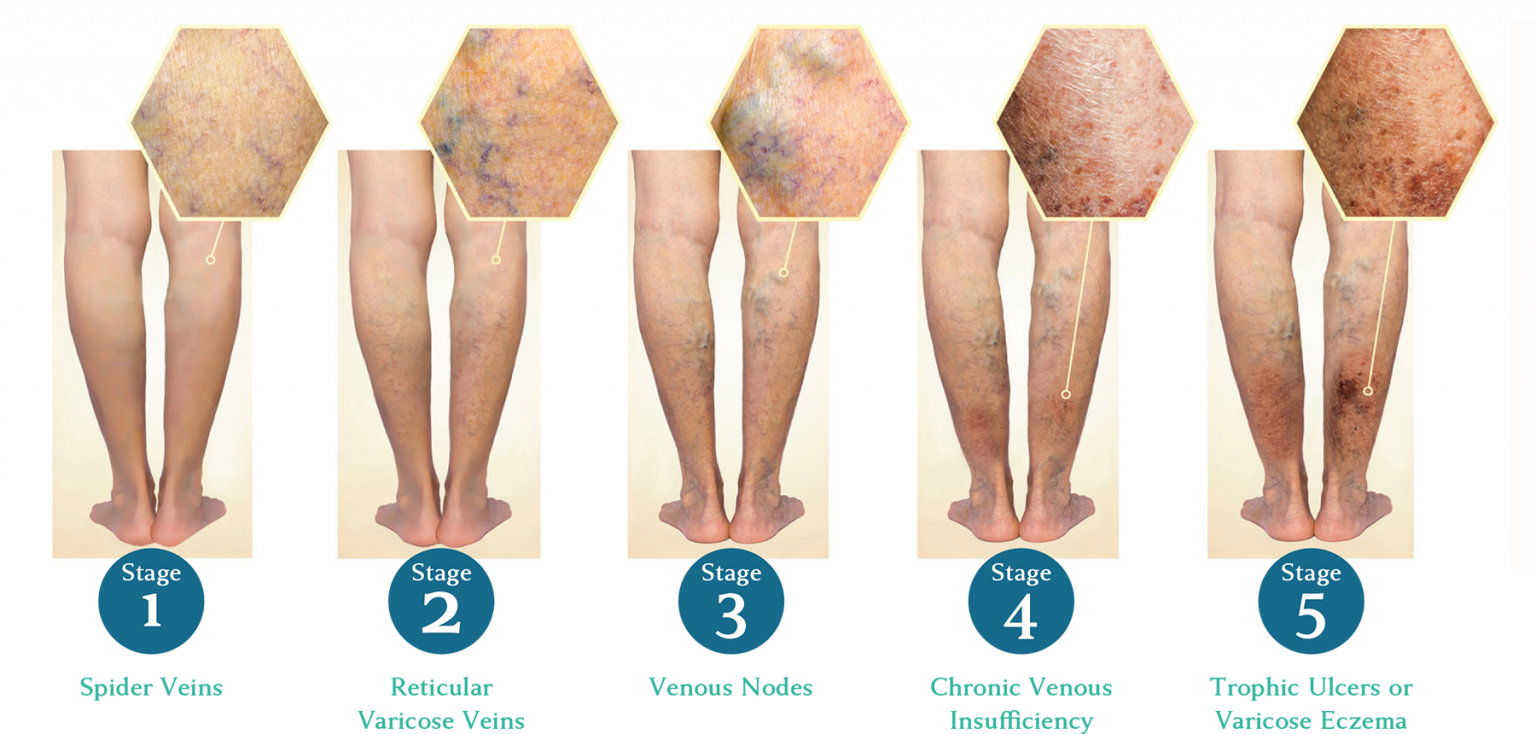
 venous disease is progressive and worsens over time.
venous disease is progressive and worsens over time.