Complications of Untreated Varicose Veins
Nisha Bunke2021-06-14T20:00:18-07:00Varicose veins and their underlying cause, venous reflux disease can cause a wide array of symptoms, including leg pain, swelling, aching, heaviness, restless legs, and nocturnal leg cramps.
If left untreated, superficial venous reflux disease can progress to cause skin changes and other complications.
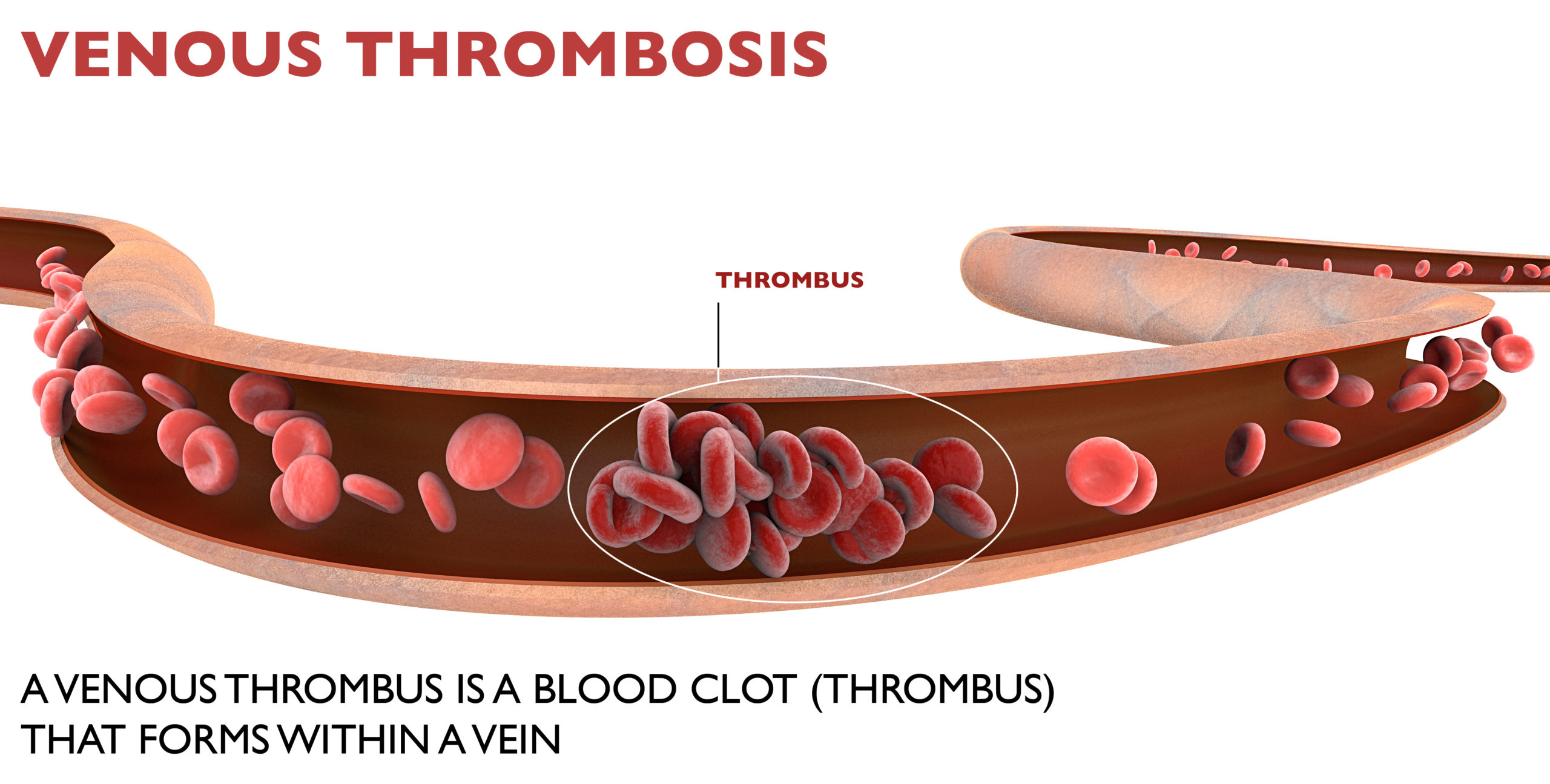
Complications of untreated venous disease include:
1. Superficial Thrombophlebitis (STP)
A […]