Eating for Healthier Veins
Nisha Bunke2020-08-19T00:45:26-07:00Foods that are rich in flavinoids may improve symptoms of venous disease. Flavonoids help protect plants from environmental toxins and help repair damage. They can be found in a variety of foods, such as fruits and vegetables. When we eat foods rich in flavonoids, it appears that we also benefit from this “antioxidant” power. In addition […]




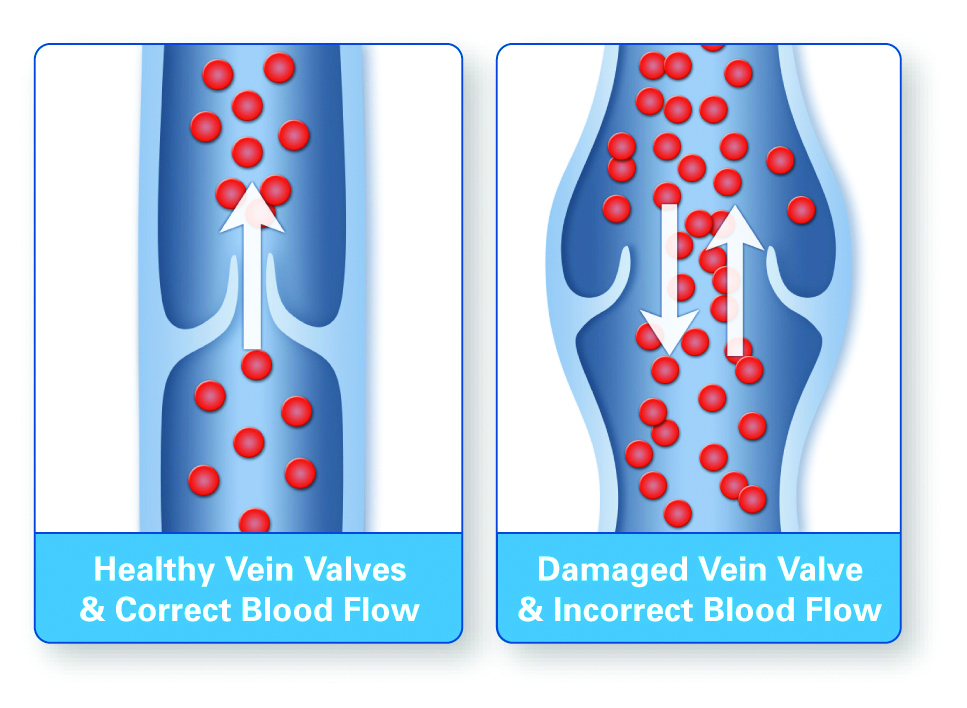
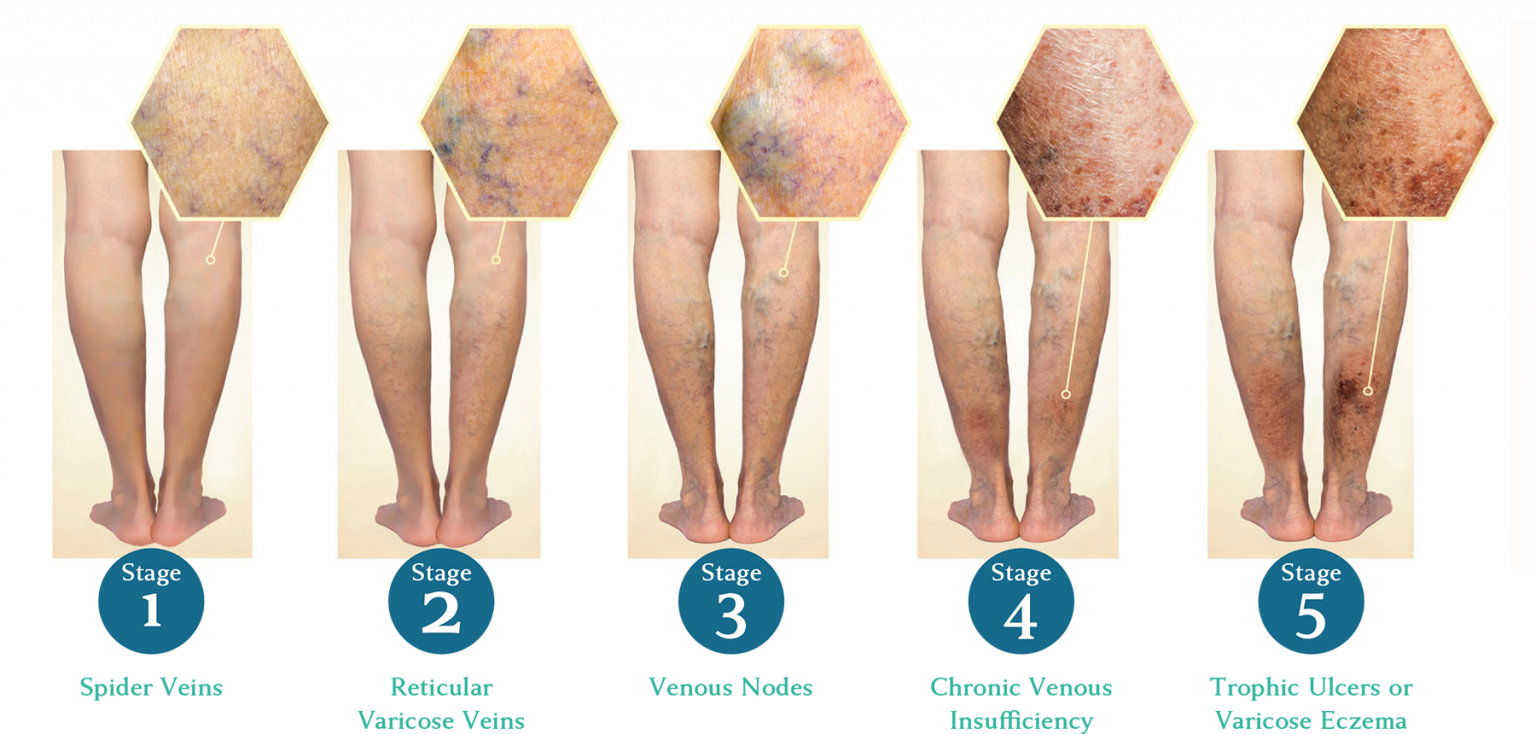
 venous disease is progressive and worsens over time.
venous disease is progressive and worsens over time.