How Laser Vein Ablation Works to Treat Varicose Veins
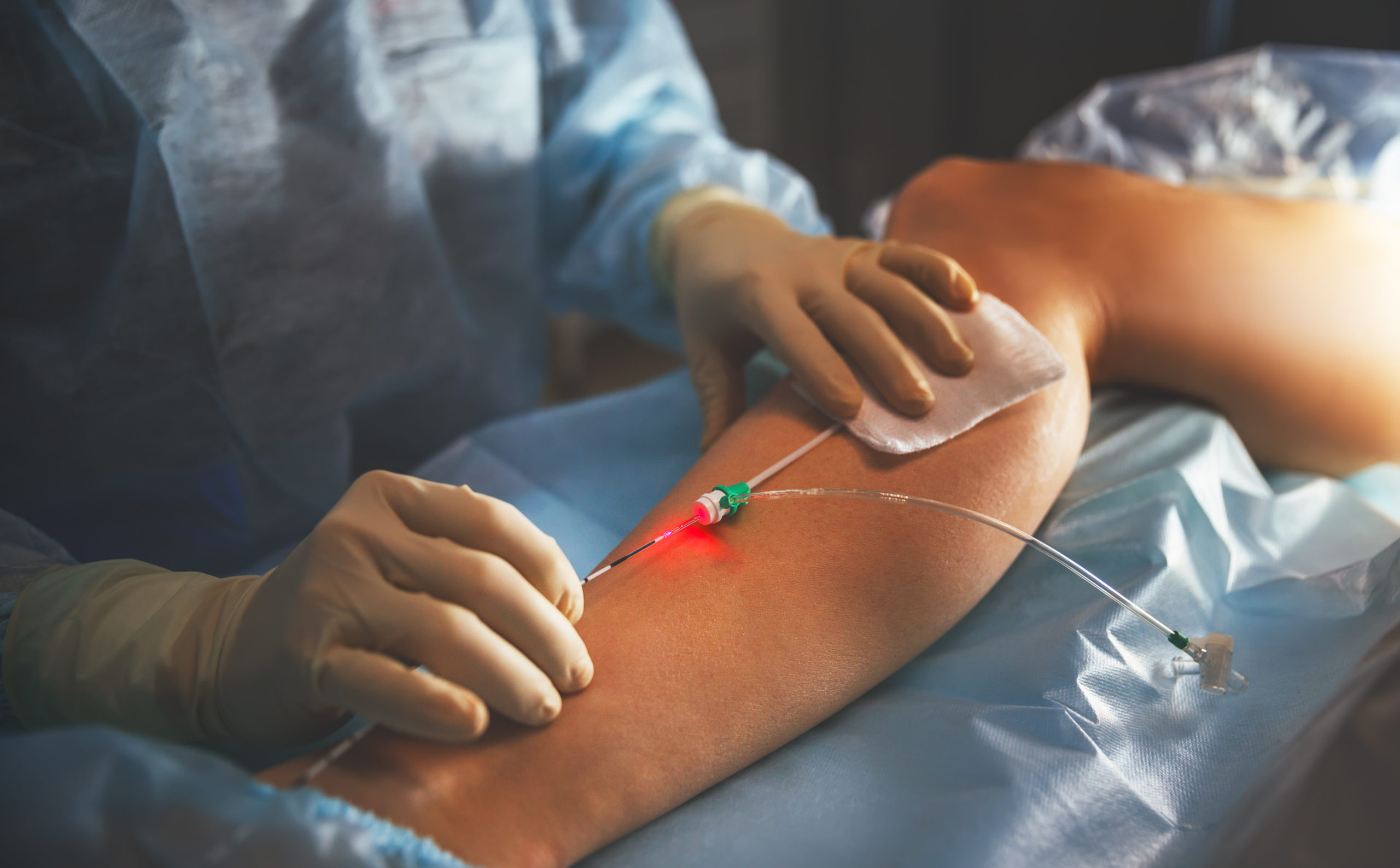
Nisha Bunke2021-06-07T13:47:35-07:00The VenaCure EVLT procedure is minimally-invasive and can be performed in a doctor’s office. It addresses both the cosmetic and medical issues associated with varicose veins.
A laser light emitted through a thin fiber inserted into the damaged vein delivers just a small amount of energy, causing the malfunctioning vein to close and seal shut.
Veins that are treatable with the VenaCure EVLT system are superficial veins. Laser therapy with the VenaCure EVLT system is indicated for varicose veins and varicosities with superficial reflux of the Greater Saphenous Vein, and in the treatment of incompetent refluxing veins in the superficial venous system in the lower limb.
After the VenaCure EVLT procedure, your body will naturally route blood flow to other veins.
Bulging and pain in the damaged and now-sealed vein will subside after the procedure.
Because VenaCure EVLT vein treatment eliminates varicose veins where they start, the results can be obvious right away.
Before undergoing any treatment, it is important to discuss with your physician the risks, benefits and alternatives to the procedure.
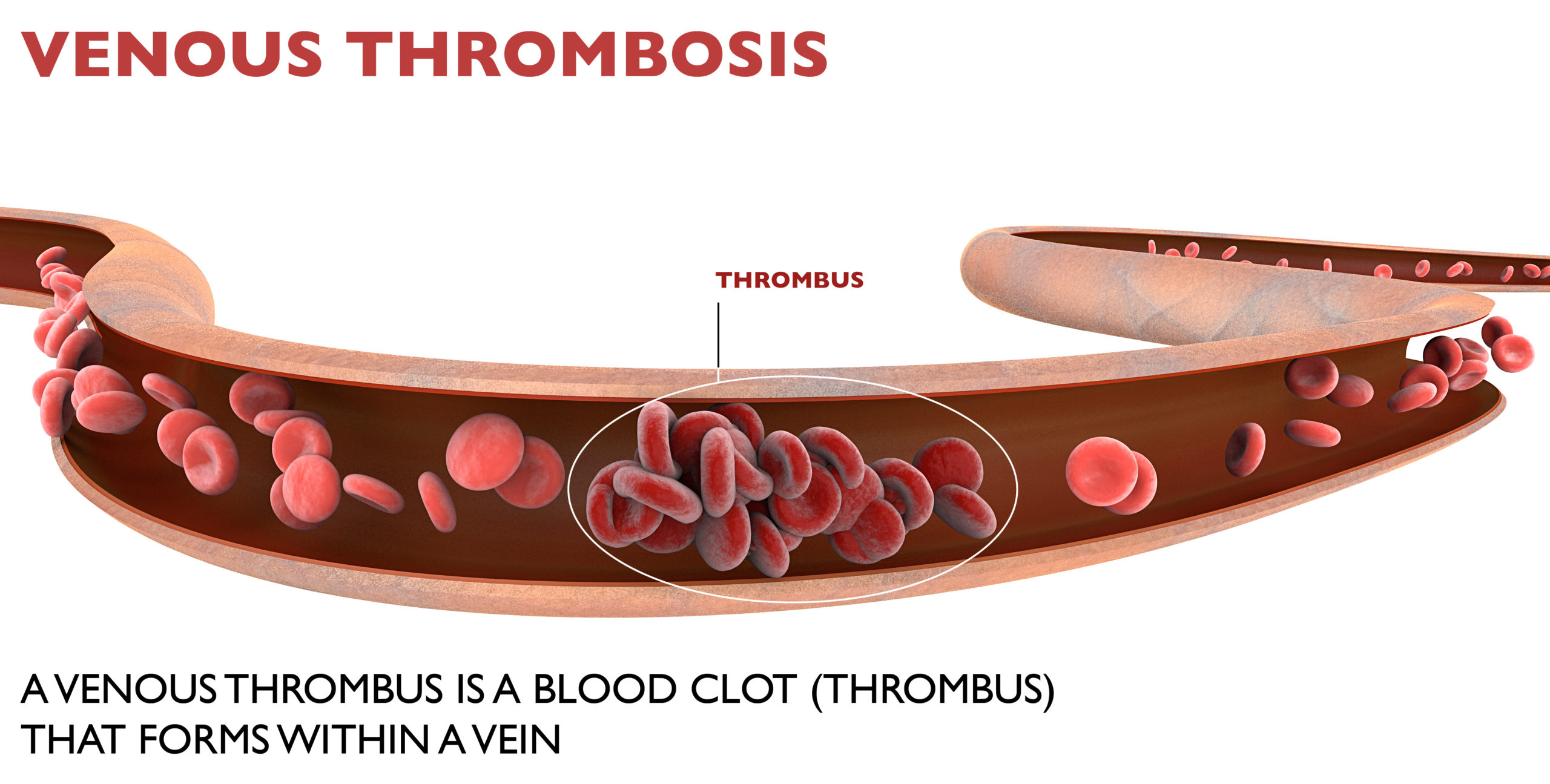
Complications with vein treatments are rare, but you should be aware of Potential Complications:
Potential complications include, but are not limited to the following: vessel perforation, thrombosis, pulmonary embolism, phlebitis, hematoma, infection, skin pigmentation alteration, neovascularization, paresthesia due to thermal damage of adjacent sensory nerves, anesthetic tumescence, non-target irradiation, hemorrhage, necrosis, DEHP exposure, skin burns and pain.
To read more about the VenaCure EVLT procedure that we perform at La Jolla Vein Care, click here. To schedule a consultation or telemedicine visit with one of our physicians to further discuss laser treatment and alternatives to laser, call us at 858-550-0330.